Roberto Italo Tozzini
Anatomy and Physiology of the Female Genitalia.
External Genitalia: Vulva
As external genitalia we can distinguish, between the genito-crural furrows, the Vulva, which extends upwards and forwards with the Mount of Venus and that below and behind, after the hairpin, continues with the perineum that separates it from the anus.
In the vulva we describe: the clitoris, the labia majora and minora, the vulvar fork and, in a deeper plane, the vestibule that shows the mouth of the urethra to the front and back, the hymen or the vaginal introitus.
-
Clitoris. It is the equivalent of the penis in the male. It consists of two corpora cavernosa ending in a small glans. The corpora cavernosa attach to the ischiopubic rami and then unite in the midline. They are covered by a cutaneous fold that is a continuation of the upper branch into which the lower lip is divided upwards and is called the cap, while the lower branch of this division is fixed to the ventral face of the clitoris, constituting the frenulum.
-
The labia majora are cutaneous folds that laterally limit the vulva, covering the labia minora and hiding the vaginal entrance or introitus. It contains an adipose filling that extends upwards with the fat pad of the mons pubis and shows sexual hairs on its outer side, while, on the inner, hairless side, numerous sebaceous and sweat glands flow, producing a characteristic odor. Towards its lower end, it joins the opposite side in a kind of fold called the vulvar fork. Further back, the perineum separates it by about 2.5 cm from the anal opening. The labia majora are separated from the labia minora by the interlabial sulcus.
-
Minor lips. Also known as Nymphs, they are thin skin reeds of variable length that protect the vaginal introitus and the urethral meatus. Sometimes they can reach considerable development. It does not have hairs, but it does have sebaceous glands and inwards, in the nipho-hymenal sulcus that separates them from the introitus, the Bartholin glands flow, the most important of which provide lubrication with their secretion during sexual arousal and intercourse.
- In the vestibule, located in a deeper plane than the nymphs, an anterior orifice or urethral meatus is observed and, backwards, the entrance of the vagina or introitus, which in the virgin woman is partially covered by a highly vascularized connective tissue membrane. called hymen. After the beginning of penetrative sexual activity, the hymen tears, persisting remains of tissue in the form of fringes, called myrtiform caruncles.
Internal Genitalia Vagina
It is an extraperitoneal intrapelvic organ consisting of a muscular duct lined by stratified mucosa, flattened from front to back and extending from the introitus to the cervix, going up and back in the pelvis, towards the sacrum. The vagina at rest, measures on average about 8 cm, the length of its posterior side being greater than the anterior and during intercourse its elongation occurs, reaching 10-12 cm.
At its upper end, the vagina inserts around the cervix, generating a circular space called cul-de-sac. The posterior, more pronounced, contacts the most declining area of the peritoneal cavity, called the cul-de-sac of Douglas. On its way to the external genitalia, the vagina makes contact on its anterior face, first with the bladder and then with the urethra, which rest on the vesico-vaginal septum. Behind, the recto-vaginal septum separates it from the rectum, up to its terminal portion where a fibro-muscular nucleus called the perineal wedge intervenes, which tends to tear during childbirth, contributing to the presentation of prolapses.
Uterus . Outside of pregnancy it is a hollow viscus with a virtual cavity (endometrial cavity), the faces of which remain attached. In this partially intraperitoneal organ, 3 segments with different structure and functions are distinguished: the cervix, the isthmus and the uterine body.
The cervix, as we have seen, is inserted into the vaginal apex, giving rise to the anterior, lateral and posterior cul-de-sac, is extraperitoneal and has a central canal or endocervical canal of about 25 mm in extension that communicates the uterine cavity with the environment vaginal. The ectocervix, like the vagina, has a mucosa with stratified epithelium without a corneal layer and the endocervix, a columnar epithelium with ciliated and mucous-secreting cells. Both mucous membranes converge at the level of the external cervical os, although depending on the physiological circumstances this area may move towards the external surface (childbirth) or into the canal (menopause). Being an epithelial transition zone, with frequent necrosis and re-epithelialization,
The adult uterine body, in nulliparous women, measures internally about 5 cm in length, has an intercornual width of 4 cm, and is slightly triangular in shape with its base facing the abdominal cavity. It consists of 3 layers, the internal or endometrial mucosa, with a superficial or functional layer that is renewed with each menstruation and a deep, fixed basal layer that allows the renewal of the mucosa after each menstruation. The endometrium is a tissue highly sensitive to ovarian hormones and estrogens produce an active pattern of proliferation with glandular growth and vascularization of the stroma, while progesterone, increasingly secreted from ovulation, it inhibits endometrial action and determines characteristic secretory changes in the epithelium and stroma (decidual cells), preparing this mucosa for the implantation of the embryo. If pregnancy does not occur, both steroids decrease rapidly by activating matrix metalloproteinase type enzymes and the vascular system where intense vasoconstriction will occur, determining the sum of factors necrosis, disintegration and expulsion of the functional endometrium with menstrual blood. .
The muscular layer has a great development and its contraction favors the expulsion. It shows a remarkable capacity for distension during pregnancy and its contractions are activated during childbirth or abortion. The peritoneal serous finally covers the entire peritoneal surface of the viscus. In front, it separates it from the bladder to the vesico-uterine cul-de-sac and behind it, it surpasses the posterior aspect and the neck to constitute the cul-de-sac of Douglas, adjacent to the posterior cul-de-sac of the vagina. Laterally it extends to the pelvic wall, allowing the transit of the uterine vessels that enter and exit the uterus and upper third of the vagina and the passage of a strong uterine attachment ligament to the center of the pelvis; the cardinal or Mackenrod ligament. These peritoneal folds, They are known as Broad Ligaments and they highlight the round ligament, the fallopian tube and the utero-ovarian ligament from front to back. At the base of this peritoneal tent, the aforementioned cardinal ligament is located and, outside and behind the arch of the uterine artery, it crosses the ureter on its way to the bladder. Between the body and the cervix, there is the point or the narrowest area of the uterus, with circular musculature and a mucosa that is not very receptive to hormonal stimulation, which is called the uterine isthmus, with retention functions during pregnancy. it crosses the ureter on its way to the bladder. Between the body and the cervix, there is the point or the narrowest area of the uterus, with circular musculature and a mucosa that is not very receptive to hormonal stimulation, which is called the uterine isthmus, with retention functions during pregnancy. it crosses the ureter on its way to the bladder. Between the body and the cervix, there is the point or the narrowest area of the uterus, with circular musculature and a mucosa that is not very receptive to hormonal stimulation, which is called the uterine isthmus, with retention functions during pregnancy.
The fallopian tubes , or oviductsThey are tubular in structure and measure 10 to 12 cm long, with an internal diameter that increases from the uterine horn (1 mm) to its termination in the ampulla and fimbriae (1 cm or more). It has an intramural portion of cm, the isthmus of about 3 cm and the pavilion of 4 to 8 cm where its lumen becomes wide, ending in mucous fingerings, called fimbriae, that are applied to the ovarian surface at the time of ovulation. One of them, the Ovarian Fimbria, remains in stable contact with the gonad. In the ampulla, the fertilized egg expels its second polar corpuscle and begins to actively divide. After 4 to 6 days, it reaches the endometrial cavity in a morula state to start the implantation process. The interior of the tubes is lined by a ciliated columnar epithelium,
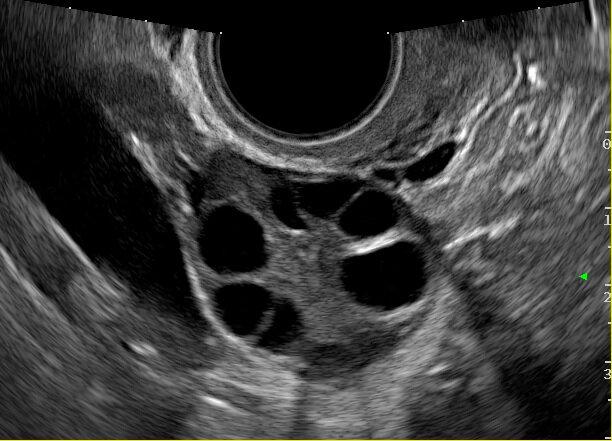
the ovaries. The female gonads include two similar glands located laterally in the pelvis, behind the posterior sheet of the broad ligament and in contact with the fimbriae of the oviduct. At its antero-inferior end, it joins the uterus through the utero-ovarian ligament and at its upper end, receives its main supply from the ovarian artery that comes from the aorta or the left renal artery and passes through the infundibulum-pelvic or suspensor ligament. of the ovary. The gonad is about 3 to 4 cm long by 2 wide and 1 cm thick, with a volume of about 6 cm3. It shows the cut, a cortical zone, where the follicles nest in their different evolutionary states: primordial, primitive, secondary or antral, mature and ovulatory. All follicles originate during embryonic life; they are around 1,000,000 at birth, to be reduced to about 250,000-300,000 at the time of menarche and <2000 when menopause is reached. During reproductive life, only about 500 follicles ever ovulate. Inside the cortex is the medulla, rich in vascular and loose connective elements.
The follicle is the functional unit of the ovary since it combines hormonal and gametogenic activity. In its interior and commanding its development, is the ovule or female gamete with 23 chromosomes, but stopped in prophase of its first meiotic division. The ovum is surrounded by nurse cells, responsible for metabolic exchanges, called cells of the radiated crown. On the outside, between the "antrum" or space filled by the follicular fluid, there are several layers of epithelioid cells, called granulosa cells, a true transitory powerhouse in the production of estrogens, HAM, various proteins, peptides, cytokines and the follicular fluid itself. . They have receptors for FSH, which is the main motor of follicle development, and in their maturity stage, they also acquire receptors for LH. Around the granulosa cells there is an anhistic collagen membrane to which vessels and innervation reach without penetrating it and outside of it other cells of conjunctival lineage differentiate into epithelioids, rich in lipids (LDL cholesterol) with receptors to LH, called, cells of the theca interna and that appear from the secondary antral follicles. These cells manufacture androgens (androstenedione, testosterone and DHEA) part of which act on effectors such as the hair follicle and part diffuses into the follicle to be metabolized into estradiol in the aforementioned granulosa cells. The external teak has a less defined structure and function and becomes progressively confused with the adjacent tissue. In some species, you have smooth muscle fibers, apparently linked,
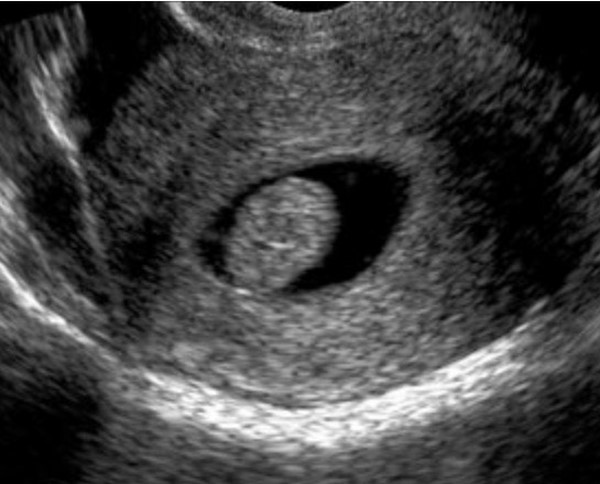
From the functional point of view, the follicle is characterized by its cyclical activity, maturing under the action of gonadotropins from its antral development, with increasing production of estradiol by the granulosa that activates its aromatases enzymes, until reaching a value maximum or peak (around 250 to 350 pg / ml of estradiol) which in turn produces the surge of LH (LH peak by feed back + E2) from the pituitary gonadotropes and this, reactivates the first meiotic division of the ovum, produces ovulation and determines the formation of the yellow body. The corpus luteum or corpus luteum, now replaces the follicle, being a solid, highly vascularized structure, composed of luteinized cells of the granulosa and theca interna that secrete increasing amounts of progesterone and constant amounts of estrogens, necessary to prepare the endometrium and other tissues for the implantation of pregnancy. If there is no gestation, the corpus luteum returns after 12-14 days and a new cycle begins; if there is, the HCG produced by the embryo will keep that corpus luteum gravidarum active for about 8 more weeks, when the placenta will take metabolic and hormonal control of pregnancy.
|
Table 1 Main reasons for consultation in Gynecology.
|
THE GYNECOLOGICAL CONSULTATION. Questioning or anamnesis.
The interrogation marks the beginning of the medical consultation, being of fundamental importance to guide the diagnosis, appreciate the potential risks to the health of women and develop a solid doctor-patient relationship. It should be friendly, concise, and complete.
The data collected, dumped on a sheet of paper or in a computer program, constitute the Clinical History of the patient and summarize the family and personal history and the sociocultural environment in which it develops its activity, as well as its symptoms and signs and possible diagnoses, constituting an essential tool for the evaluation and follow-up of healthy or sick women, as well as an unavoidable document due to its medico-legal value, in multiple circumstances. This information will allow us to locate the woman in her condition and circumstance, as being psychobiosocial and therefore, resulting from the interaction of her genomic structure with her environment, including the intestinal microbial presence or microbiome, which ends up generating special circumstances for each person.
Strictly gynecological, this questioning will look for a family history of cancer (mammary-ovarian) and hereditary diseases linked to the genital sphere or of female prevalence. On a personal level, breast and pelvic diseases and surgeries will be investigated, the performance or not of Papanicolaou studies and mammograms if they fit, the application of HPV vaccines and the existence of addictions such as smoking, drug addiction or alcoholism. The age of menarche or sexual development, the characteristics of the menstrual cycle or the date of the last menstruation should be recorded if you are in menopause. If you have sexual intercourse with or without contraceptive care and, fundamentally, if you have become pregnant, how many times and how have your deliveries and lactations or abortions been. If you are in menopause, You must record if you are or have performed hormonal treatment and what it has consisted of. The gynecological examination must be complete, including inspection of the external genitalia and secondary sexual characteristics, adequate palpation of the internal genitalia (except in virgins), and examination of the breasts. Blood pressure measurement should also be included in adult women.
REASONS FOR CONSULTATION.
|
Table 2
|
Apart from the health consultation, which is becoming more and more frequent and is carried out for preventive purposes, women usually consult for any of the following symptoms (Table 1).
Of course, these reasons for consultation must vary according to the age and reproductive stage of the patient (girl, pubescent, adolescent, adult or post-menopausal). This chapter is focused on the adult patient, so we will mention only some of the most common conditions. highlights that are observed from the date of menarche.
Alterations of the menstrual cycle. The normal or eumenorrheic menstrual cycle presents the following characteristics: duration, 28, + - 7 days; menstrual flow lasts 3 to 7 days with an estimated blood loss of 20 to 60 ml and is accompanied by a feeling of minor pelvic discomfort that does not interfere with normal activity.
The cycle can be altered in its frequency: if it is shortened, (<21 days) it is referred to as polymenorrhea or frequent bleeding (FIGO 2011); if it is prolonged, between 36 and 89 days, it is defined as oligomenorrhea or infrequent menstrual bleeding (FIGO 2011). After 90 days without bleeding, the patient is amenorrheic. In turn, menstrual flow can last for more than 7 days and is thus expressed according to FIGO (prolonged menstrual bleeding), replacing the term menorrhagia and if it is shortened, defined as hypomenorrhea (2 days or less), FIGO expresses it simply as "short menstrual bleeding". The term hypermenorrhea is reserved for very heavy menstruation (Table 2). In general, these cycle changes, a frequent reason for consultation in young women and adolescents, only reflect alterations in the ovarian cycle, at a central level (stress, excessive weight loss regimes) or intrinsic gonadal (PCOS). It was mentioned that the cycle may also be absent (amenorrhea) and this occurs after more or less normal menstruation (secondary amenorrhea), adding to the aforementioned central, gonadal and endocrine causes that alter the cycle, normal or pathological pregnancy in women with sexual intercourse. Also endometrial diseases or hysterectomy can produce this symptomatology. If you have never menstruated, we are facing a primitive amenorrhea that will also be of central cause (hypothalamic-pituitary, with low gonadotropins) or gonadal (with high gonadotropins), here being frequent genetic alterations (dysgenesis) or due to the absence of the effector ( uterus vaginal agenesis). In some genital malformations,
The presence of bleeding outside of menstruation is called metrorrhagia or spotting or dripping if it is minimal, but in the nomenclature accepted by FIGO (2011) it is mentioned as SUA (abnormal uterine bleeding) The different pathologies that can be expressed with abnormal bleeding They are read in Tables 3 and 4. Finally, on premenstrual days, due to the action of the progesterone secreted by the corpus luteum, some breast tension, slight weight gain and pelvic discomfort may occur. The exaggeration of these sensations is called mastodynia at the level of the breast and dysmenorrhea with or without premenstrual syndrome in terms of the ovarian cycle. If this situation produces emotional lack of control, the "premenstrual dysphoric disorder" is added to the premenstrual syndrome.
The pain , partially quoted, is another common cause of gynecological consultation. It can present in an acute form and be a single episode or recur with certain periodicity, associated or not with menstrual episodes. It can also be chronic, persistent, unrelated to menstruation or related to the cycle. Ectopic pregnancy, adnexal torsion, genital malformations with cryptomenorrhea, endometriosis, adnexal infections (pyosalpinx and ovarian abscess), chronic pelvic disease, and pelvic varicocele are listed as causes of this symptomatology.
Many consultations are for genital dischargein sexually active women. Vulvar itching, which is particularly bothersome in patients with candida albicans infection, can be added to the sensation of vaginal moisture and discharge. In these cases, the discharge is white, thick, odorless and adherent to the vaginal mucosa and often occurs during pregnancy or taking hormonal contraceptives or after prolonged treatment with antibiotics or in diabetic women. If the flow is abundant, greenish-yellow, fluid, with little or no odor, even visualizing small bubbles with specular observation, it is likely that we are in the presence of a flow caused by trichomonas, easy to diagnose if we observe a drop of it under the microscope and we checked the presence of trichomonas, flagellates endowed with mobility. If the discharge is grayish or whitish, abundant and with a penetrating and unpleasant odor, one can think of a picture of vaginosis due to the coexistence of gardnerellas with anaerobic flora. Finally, vaginal discharge may be purulent with redness of the cervix and vaginal wall associated or not with symptoms of infection (gonococcia). The laboratory confirms, in all cases, the clinical suspicion.
Post-menopausal metrorrhagia; already considered generically, it takes on special relevance when it occurs in post-menopause. In such circumstances, it is necessary to confirm or rule out the diagnosis of endometrial carcinoma. Transvaginal ultrasound, hysteroscopy or biopsy curettage of the endometrium will be used for this. Also SUA should be investigated when it appears after sexual intercourse or is maintained over time, in a woman of reproductive age, who does not perform periodic controls or Pap smears. The single placement of the vaginal speculum can lead to a carcinoma of the cervix.
Breast tumorThe alterations of the mammary gland result in iterative consultations, generally associated with the fear of the diagnosis of cancer. Under the age of 30, breast cancer is very rare and most solid tumors will be fibroadenomas, showing semiologically clear limits, size between 1 and 4 cm and good mobility. If the formation is cystic in nature, as confirmed by ultrasound or puncture, the mobility will be less, as well as the consistency, it can appear in a short time and the breast will present firmer areas, typical of a fibrocystic mastopathy. Any breast tumor that occurs after age 40 deserves a thorough examination to confirm or not the diagnosis of cancer. Although the semiology is helpful (high consistency tumor, irregular borders, adhesions to skin or neighboring tissues, etc) an early diagnosis is intended, only possible by imaging (digital mammography, simple or 3D, simple ultrasound or color Doppler, MRI) and in suspected cases, stereotaxic directed core biopsy (mamoton or suros). On the other hand, breast pain has little relevance, except in acute infectious processes related to breastfeeding (mastitis or breast abscesses) and discharge from the nipple, it is an infrequent symptom and except for the presence of blood in it, typical of benign pictures of the gland.
Other reasons for consultation are read in Table 1, requiring in each case its own diagnostic methodology.
STUDY METHODS
|
|
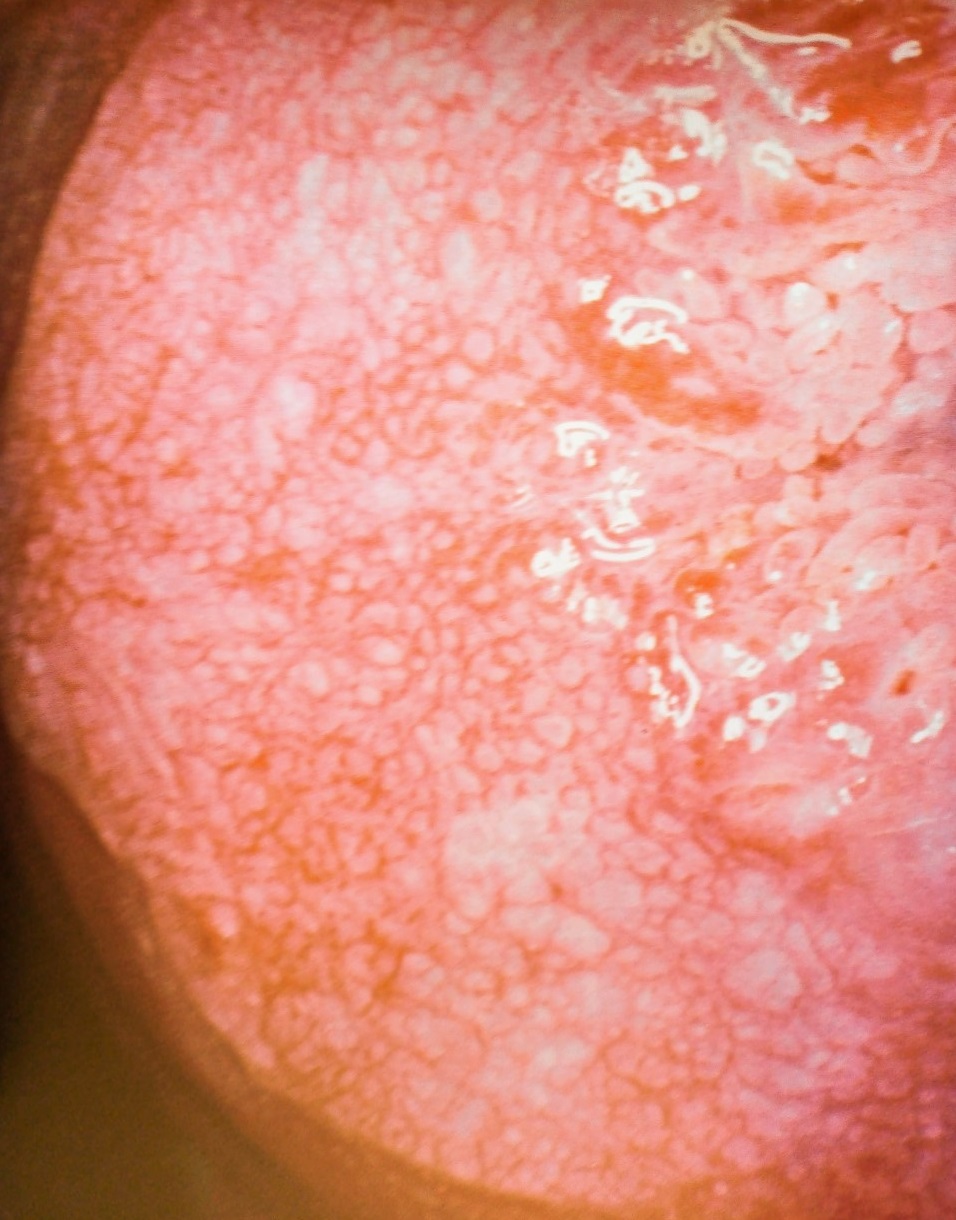

Figure 7 and 8: Colposcopic images of mosaic and red spots corresponding to low-grade intraepithelial lesion
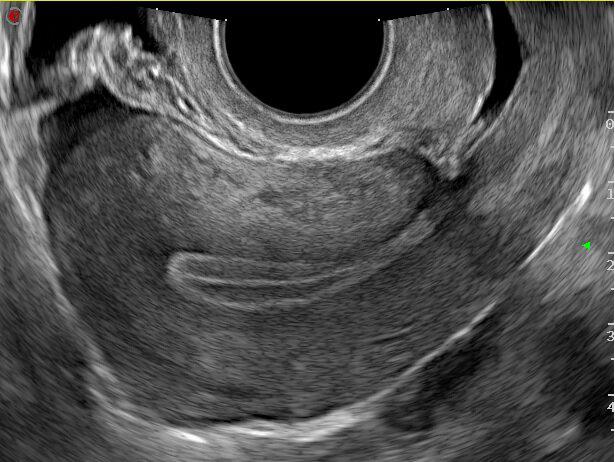
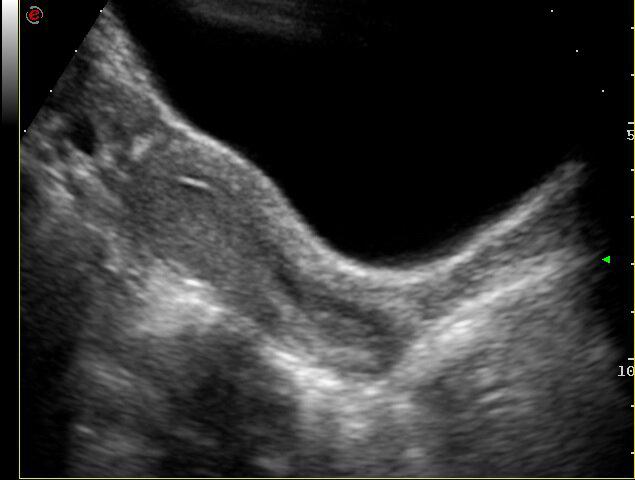
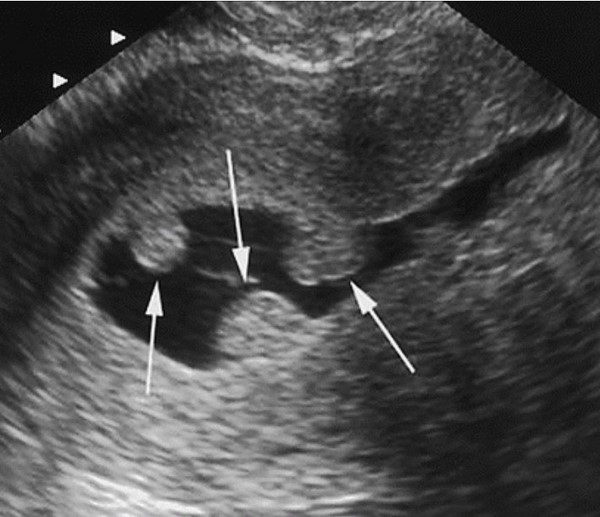
The advances in this chapter are extraordinary. Well used, it can be said that very few women go undiagnosed in the case of presenting pathologies. The old "exploratory laparotomy" as a method to establish the cause of a gynecological disease has now disappeared. It is no longer conceivable to operate without prior diagnosis. Continuous advances in the field of images allow us to know with increasing precision the condition of the female pelvic genital organs. Ultrasound is the first great auxiliary, almost indispensable, to assess the anatomical and functional state of the uterus and ovaries through the transvesical abdominal route in thin women without sexual intercourse or through the vaginal route, in those with sexual activity who accept this route or in obese women. where the thickness of the abdominal wall makes good visualization difficult. In Figures 1, 2, 3, 4, 5 we see examples of normal genitalia and some pathology. Today the so-called 4D technique provides excellent images, which is why it is frequently used in the morphological study of the fetus in its third trimester.
Multislice computed tomography (multislice) has made it possible to obtain high-quality images with 3D capability, although by using ionizing radiation, it interacts with living tissue and can produce undesirable effects. Of course, it is contraindicated in pregnant women.
Magnetic resonance imaging: this method is based on radio frequency waves under a magnetic field circumscribed to a specific region of the body. For better evaluation, gadolinium is used as a contrast medium. It is a highly anatomical method especially in the T2 sequences, allowing to differentiate inflammatory processes from tumor ones and with gadolinium benign cancer tumors. It is also essential for the study of malformations and DDS (Disorders of Sexual Development)
PET-CT: it is a proton emission tomography (PET) combined with a multi slice tomography. They are two teams together, although the patient performs the study on a single stretcher. PET uses a radioisotope administered intravenously (18-Fluor-Deoxyglucose) that is taken up by all tissues, but with accumulation in those that show a high number of mitoses. This makes it possible to locate neoplastic lesions anywhere in the body as long as they reach a certain volume (mass greater than 1 cm in diameter). PET-MR uses MRI instead of tomography, but its use in our environment is still very limited.
Watch video about gynecological laparoscopy
Endoscopic images: since the 70s, pelvic endoscopy began a progressive development that has transformed it into an indispensable tool, not so much for diagnosis (as it was originally) but for surgical treatment, with high-resolution video laparoscopy and 3D and finally, Robotics (figure 6) and video. Hysteroscopy has also seen an increase in its use as a diagnostic and therapeutic tool thanks to recent advances in technology. The uterine cavity and ostiums can now be seen in great detail and rapidly. Finally, it is worth mentioning as a study method the video colposcopy that supplies and records images of the ecto and part of the endocervix to establish the normality or not of the cervical tissues, particularly, the so-called transformation zone,
The constant improvement of the hormonal laboratory with determinations in blood at the level of picograms and fentograms, of new proteins, peptides, cytokines, tumor markers (in breast and colon cancer, for example), genomic platforms for the identification of specific mutations and polymorphisms, metabolomics and microbiome studies, etc., have drawn a new scenario, partially applicable in gynecology, called "evidence-based medicine". You do not abandon art in medical practice, but science has taken the lead.
|
Table 3
|
|
Table 4
|