by Alberto J. Muniagurria and Eduardo Baravalle
They include pulse, blood pressure, respiration, temperature, weight and height, and habit.
PULSE
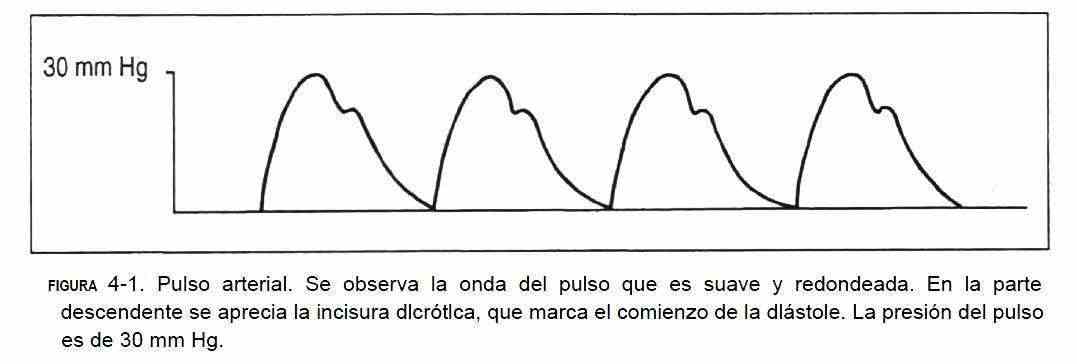
The volume of blood ejected at each ventricular systole produces a pulse wave in the arterial tree, called the arterial pulse (Figure 4-1).

Certain pulses are tested routinely, and others only selectively in certain patients. Its examination includes inspection, palpation, and auscultation. In children under 2 years of age, the brachial and femoral pulses are palpated; in older children and in young people the carotid and radial pulses are added; In the elderly, the carotid, subclavian, aorta, femoral, posterior tibial, and pedial arteries are palpated. Auscultation in children is of interest in the supraclavicular fossa, whereas in adults and the elderly the carotid, subclavian, aortic, and femoral arteries are auscultated.
 The patient should be in the supine position and the observer in a comfortable position to focus full attention on the pulse waves. The radial pulse is found at the lower extremity of the forearm, on the radial slide (Figure 4-2), located on the outside of the forearm. The ulnar pulse (Figure 4-3) is found in the lower extremity of the forearm, internally. The brachial pulse is palpated on the anterior aspect of the elbow, within the biceps tendon. The humeral pulse is sought outside the axillary cavity. The femoral pulse (Figure 4-4) is located in the inguinal crease, midway between the anterior superior iliac spine and the pubic spine. The popliteal pulse (Figure 4-5) is sought, with the knee bent and the leg relaxed, with the balls of both hands on the popliteal bone, outside the midline. It is often not found. The posterior tibial pulse (Figure 4-6) lies behind the medial malleolus of the ankle and is palpable with the distal end of the index and middle fingers. The foot pulse (Figure 4-7) is located on the dorsum of the foot, lateral to the extensor muscle of the first toe.
The patient should be in the supine position and the observer in a comfortable position to focus full attention on the pulse waves. The radial pulse is found at the lower extremity of the forearm, on the radial slide (Figure 4-2), located on the outside of the forearm. The ulnar pulse (Figure 4-3) is found in the lower extremity of the forearm, internally. The brachial pulse is palpated on the anterior aspect of the elbow, within the biceps tendon. The humeral pulse is sought outside the axillary cavity. The femoral pulse (Figure 4-4) is located in the inguinal crease, midway between the anterior superior iliac spine and the pubic spine. The popliteal pulse (Figure 4-5) is sought, with the knee bent and the leg relaxed, with the balls of both hands on the popliteal bone, outside the midline. It is often not found. The posterior tibial pulse (Figure 4-6) lies behind the medial malleolus of the ankle and is palpable with the distal end of the index and middle fingers. The foot pulse (Figure 4-7) is located on the dorsum of the foot, lateral to the extensor muscle of the first toe.
The study of the pulse includes the analysis of frequency and rhythm, amplitude and shape.
The frequency is the number of waves per minute.
Heart rate is usually determined by palpation of the arterial pulse with the ball of the index and middle fingers, usually in the radial artery. It should not be palpated with the thumb to avoid feeling one's own pulse. It is controlled with a watch, for at least 30 seconds, if the rhythm is regular; if it is irregular, the heart should be auscultated to determine the central frequency. The frequency in the normal adult is 65-85 beats per minute at rest, being higher in childhood. The increase is called tachysphigmia, and its decrease bradysphigmia.
The rhythm will be normal when the times between successive pulse waves are equal. Within normal rhythm disturbances, the presence of isolated extrasystoles should be mentioned.
The amplitude and waveform of the pulse is better palpated in the carotid due to the proximity of the heart. On inspection, the pulse waves of the carotid arteries can be observed in the neck, which, unlike the venous pulse, are seen and palpated, do not change with position or respiratory movements, and are located medial to of the sternocleidomastoid.
Rotating the head to the same side as the examined carotid, to relax the sternocleidomastoid muscle, palpate with the index and middle fingers on the inner edge of this muscle at the level of the lower half of the neck. On palpation, the pulse width is evaluated, which allows to have an idea about the stroke volume, the elasticity of the arterial wall and the ejection velocity of the blood from the left ventricle. In addition, both carotids should be auscultated (Figure 4-8). The contour of the pulse wave determines a rapidly rising wave called a percussion wave, which immediately follows the first heart sound. Subsequently, a notch called a dicrotic notch or notch is seen produced by the closure of the aortic valve, which is continued with a downward wave until the next ventricular ejection. The normal climb is smooth and fast.
Attention should be paid to changes in amplitude between wave and wave and to changes produced by respiratory movements.
BLOOD PRESSURE
Before the introduction of the sphygmomanometer, the finger of a trained observer was able to get a rough idea of blood pressure.
A mild pulse compression pressure indicates 120 mm Hg and a considerable compression pressure indicates a figure between 120 and 160 mm Hg.
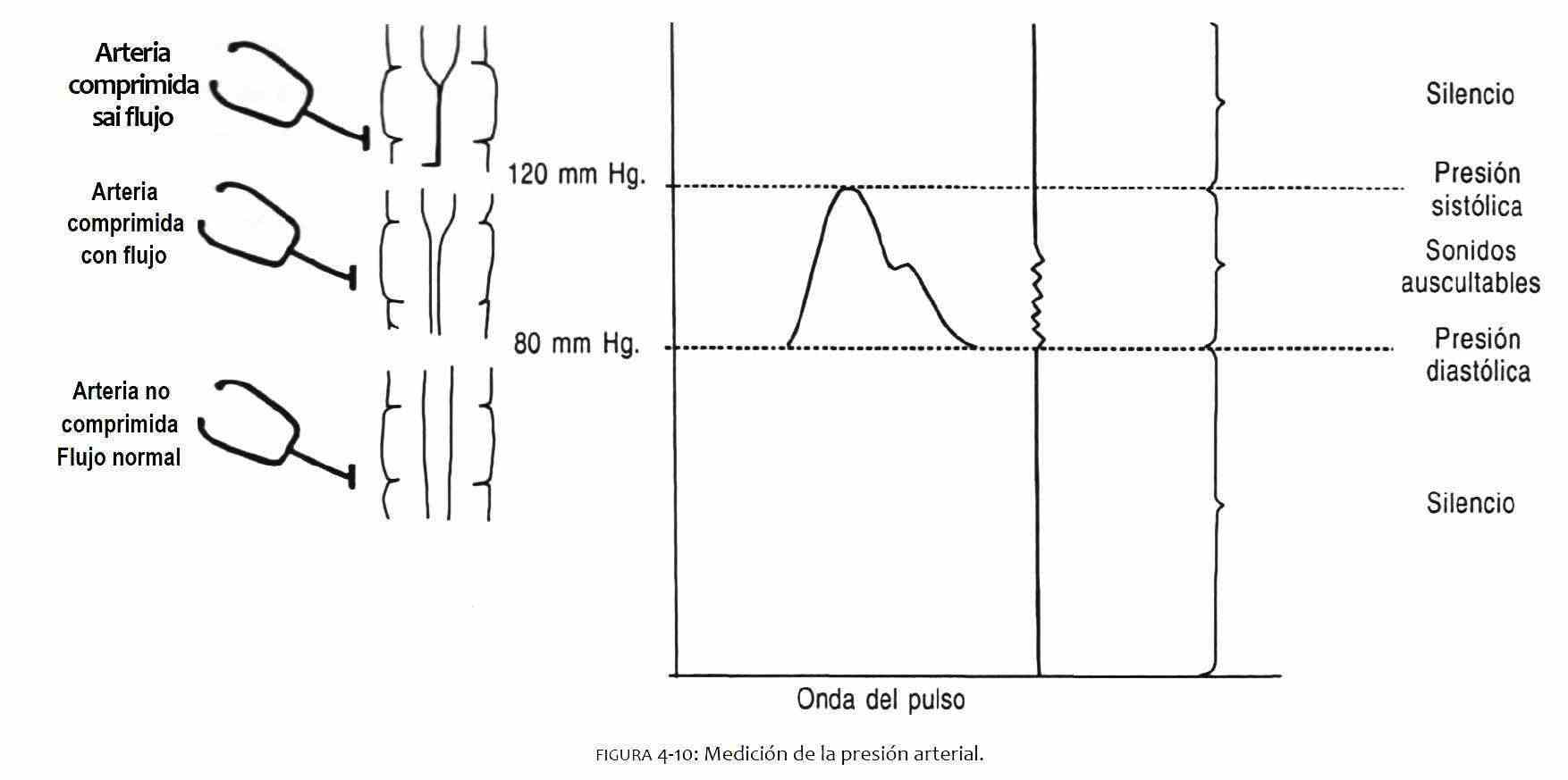
Blood pressure measurement is done with the sphygmomanometer (Figure 4-9). The sphygmomanometer has a rubber cuff covered with an inelastic material. Said sleeve is connected to the reading system and also has a rubber bulb to inflate it with a valve to later deflate it. The width of the cuff should be 40% of the circumference of the arm, while the length should be 80% of the circumference of the limb.
The aneroid sphygmomanometer should be checked periodically to calibrate its sensitivity.
Methodology . A sphygmomanometer and stethoscope are needed to measure blood pressure by the indirect or auscultatory method. The patient should be supine with the arm at heart level. In the first control, blood pressure will be measured in both arms, and also in the sitting position and in the standing position. In adults, the blood pressure in the right arm tends to be 15 mm Hg higher than in the left arm.
When standing up, the systolic blood pressure drops 5-15 mm Hg, accompanied by a slight increase in diastolic pressure, which occurs due to the increase in frequency.
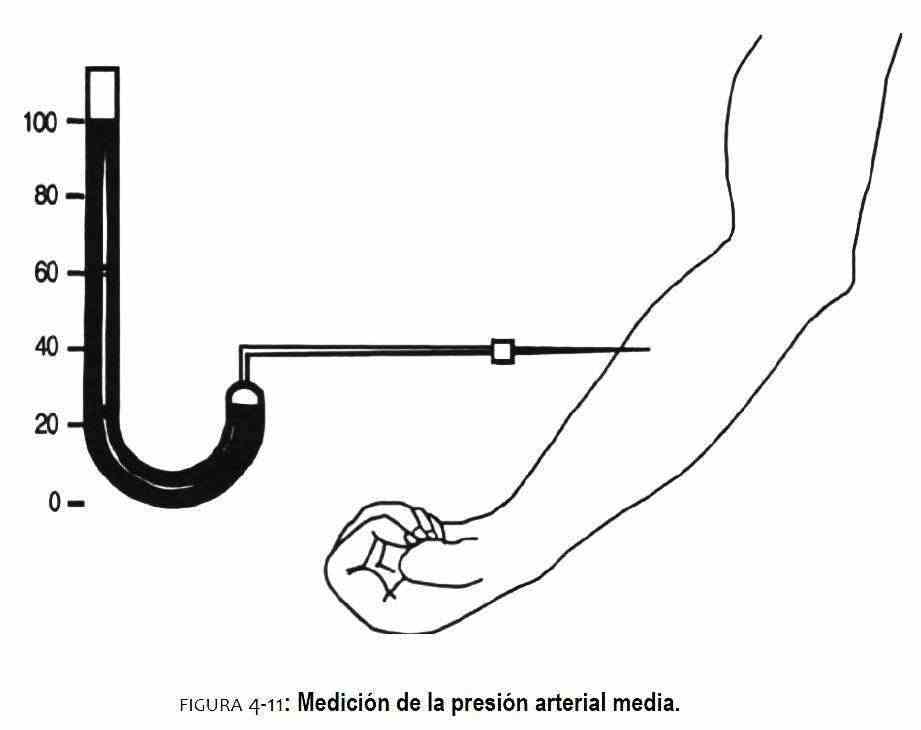
The cuff is placed at arm level, a few centimeters above the elbow crease, taking special care that it does not bulge. Air is blown into the plastic bag through the insufflation bulb, and thus the pressure from the cuff is transmitted to the arm compressing the artery. With the other hand, the brachial pulse is palpated inside the biceps tendon. The cuff pressure is raised to 20-30 mm Hg above the point where the arterial pulse disappears. Once this maneuver has been performed (Figure 4-10), the cuff is slowly deflated until the appearance of the first beat, which will mark the palpatory systolic blood pressure; in this way the so-called auscultatory pit is avoided (see Chapter 16). Subsequently, the membrane of the stethoscope or the bell (it is a low sound) is placed over the brachial artery and the cuff is re-inflated above the palpated systolic pressure. We begin again and slowly to deflate the maguine, to listen to the so-called Korotkoff noises. The first noise represents the systolic blood pressure, while the muffling or disappearance of the sounds corresponds to the diastolic blood pressure. Due to its reproducibility and its comparison with intra-arterial pressure studies, the disappearance of Korotkoff sounds is preferred as the time to determine diastolic blood pressure. Deflation should not be so slow as to cause venous congestion that causes a decrease in systolic blood pressure and an increase in diastolic blood pressure. If you want to take your blood pressure again, it is advisable to wait a minute to inflate the cuff again.
 The auscultatory method for determining systolic and diastolic blood pressure is not exact, but only approximate. The reasons for its inaccuracy are:
The auscultatory method for determining systolic and diastolic blood pressure is not exact, but only approximate. The reasons for its inaccuracy are:
1) the pressure of the cuff is not entirely transmitted to the arterial wall, since part of this energy is lost in the tissues of the arm; the loss is greater the thicker it is; 2) the person listening varies in their hearing capacity; This ability improves with training and practice; 3) If the cuff is not firmly applied to the arm, the rubber bag may protrude and the pressure is not transmitted evenly; 4) If the cuff pressure is lowered too slowly, it produces discomfort in the limb that can raise blood pressure.
Blood pressure can be taken in the forearm by palpating and listening to the radial artery. This measurement is performed in obese patients in whom the cuff does not cover the arm. It can also be measured in the lower limb. The popliteal pulse often produces only systolic Korotkoff sounds. Blood pressure can be taken over the posterior tibial artery and over the pediatric artery. The arterial pressure auscultated in the femoral artery is 10 mm Hg greater than the intra-arterial pressure.
In children, the cuff should be smaller and more appropriate.
 Physiology . If you consider a long tube filled with water, similar to the water pipe in a family home, when you open the tap the flow of water increases the more the tap is open.
Physiology . If you consider a long tube filled with water, similar to the water pipe in a family home, when you open the tap the flow of water increases the more the tap is open.
The bobbin represents a resistance to flow; when it is closed, the resistance is absolute; in qualitative terms the resistance will be infinite. When the bobbin is fully open the resistance approaches zero. Different degrees of opening of the bobbin express qualitative degrees of resistance that will vary from zero to infinity. Therefore, the bobbin is a variable resistance. The amount of that resistance can vary over a wide range.
The tap is a peripheral resistance, understood by peripheral that is far from the center of pressure; flow is reduced when resistance increases. The resistance is inversely proportional to the radius of the tube.
Pressure . When you open the tap, the water does not drip, but is forcefully ejected into the sink. The force is transmitted by the stream of water. This force is called pressure.
The greater the pressure, the greater the force that mobilizes the water and therefore the greater the flow. In the human body, pressure is generated by the operation of a pump, which is the heart. The higher the pump output, the greater the pressure, and the higher the flow rate. Flow (F) is proportional to pressure (P) and inversely proportional to resistance (R); therefore, resistance is equal to P / F and P = FxR. In other words, the pressure can increase if the flow and / or the peripheral resistance increases. If the cardiac output increases, the blood pressure will rise if the resistance remains normal. When peripheral resistance increases, blood pressure will rise if cardiac output stays the same.
There is always pressure at the level of the arteries. The energy to produce this pressure is supplied by the left ventricular pump. Pressure in the arteries is cyclical, increasing when the ventricle ejects blood into the aorta, and decreases when the ventricle enters diastole.
 By inserting a needle into the brachial artery and connecting it with a column of mercury through a flexible tube, blood pressure can be measured.
By inserting a needle into the brachial artery and connecting it with a column of mercury through a flexible tube, blood pressure can be measured.
The weight of the mercurial column is going to exert a force. The higher the mercury column, the greater the weight or force. The pressure exerted by the blood will raise the column of mercury when that pressure exceeds the pressure of the weight of the column of mercury. The degree of the pressure force can be expressed in different terms, for example, in millimeters of mercury.
When the left ventricle contracts, the intraventricular pressure rises until it exceeds the aortic pressure, thereby opening the aortic valve and ejecting blood into the aorta and arterial system. As the ventricle continues to contract, the pressure continues to rise. This elevation is known as systolic blood pressure. When the ventricle finishes its contraction and begins to relax, the intraventricular pressure begins to decrease, until the aortic valve closes when the pressure in the left ventricle is less than the pressure in the aorta. The closing of the valve marks the end of systole.
Blood pressure can be accurately measured only if a needle or catheter is inserted into the artery (Figure 4-11). In this case, the mercury manometer attached to the needle will only measure mean arterial pressure, because the mercury column has too much inertia to faithfully follow the rapid fluctuations in pulse pressure. If the blood pressure is measured in the left ventricle and in the aorta at the same time, it will be seen that the aortic pressure does not rise until the ventricular pressure reaches a value of 80 mm Hg (Figure 4-12). The level of pressure achieved will vary from person to person depending on the diastolic pressure of the aorta. At this level, the aortic valve opens and the aortic pressure rises, thereby beginning the systolic phase of the aortic pulse pressure.
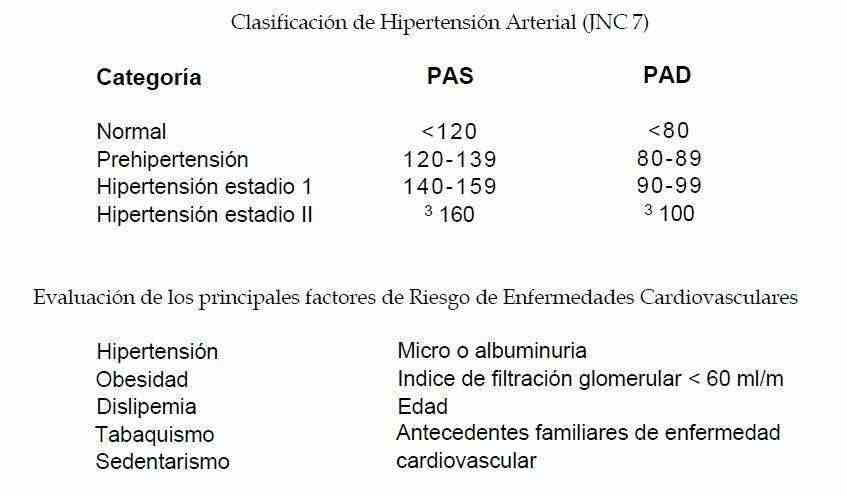
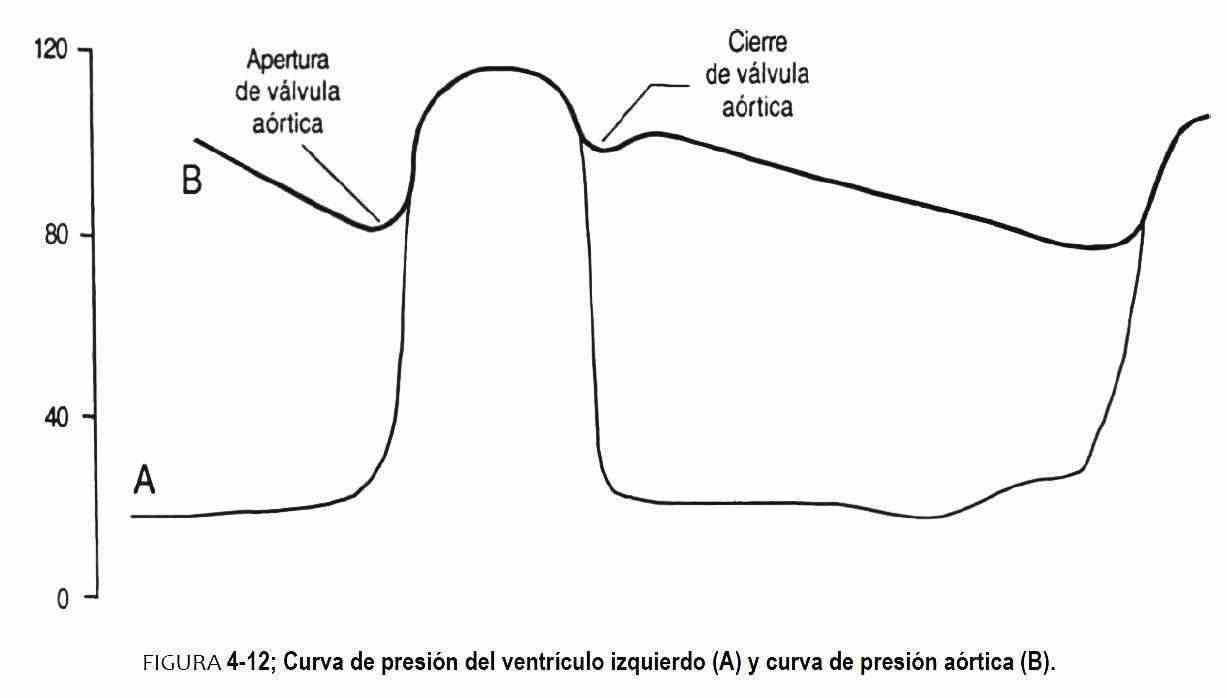 This point is the systolic aortic pressure and occurs midway through the systolic phase of the aortic pulse pressure, which in normal cases is 120 mm Hg. The aortic pressure continues in parallel with the ventricular impulse until the ventricular pressure begins to drop more rapidly than the aortic pressure. At this point the aortic valve closes and marks a small notch, called an incisura, followed by a rebound wave, known as a dicrotic wave that is inscribed in the recording of aortic pressure. Aortic pressure drops gradually as blood flows into arteries, capillaries, and veins; this pressure continues to drop until intraventricular pressure once again opens the aortic valve in a new cardiac cycle. This lower point is known as the foot of the aortic pulse pressure and represents the arterial diastolic pressure, which in normal cases is 80 mm Hg. The upper limits of normal blood pressure in adults and the elderly are <120 and <80 and 140-90 mm Hg; but the lower of these values should be considered suspicious in the case of an adolescent. Therefore, the blood pressure reading should be performed in three separate visits and interpreted according to the prior knowledge of the patient and his clinical status.
This point is the systolic aortic pressure and occurs midway through the systolic phase of the aortic pulse pressure, which in normal cases is 120 mm Hg. The aortic pressure continues in parallel with the ventricular impulse until the ventricular pressure begins to drop more rapidly than the aortic pressure. At this point the aortic valve closes and marks a small notch, called an incisura, followed by a rebound wave, known as a dicrotic wave that is inscribed in the recording of aortic pressure. Aortic pressure drops gradually as blood flows into arteries, capillaries, and veins; this pressure continues to drop until intraventricular pressure once again opens the aortic valve in a new cardiac cycle. This lower point is known as the foot of the aortic pulse pressure and represents the arterial diastolic pressure, which in normal cases is 80 mm Hg. The upper limits of normal blood pressure in adults and the elderly are <120 and <80 and 140-90 mm Hg; but the lower of these values should be considered suspicious in the case of an adolescent. Therefore, the blood pressure reading should be performed in three separate visits and interpreted according to the prior knowledge of the patient and his clinical status.
BREATHING
The pressure changes that occur in the thoracic cavity due to the contraction and relaxation of the respiratory muscles (diaphragm and intercostal muscles) produce the entry and exit of air from the airways. It is an automatic movement, controlled by the respiratory center of the central nervous system. The chest wall is mobilized upward, forward, and laterally, and the diaphragms descend during the inspiratory act. Relaxation of the respiratory muscles and elasticity of the lung produce expiration. Under normal conditions, expiration lasts twice as long as inspiration. In the normal subject, respiratory movement produces a whisper that is difficult to hear in the patient's mouth, called a white sound.
Methodology . The respiratory rate and rhythm and the inspiration / expiration ratio should be evaluated. To determine the respiratory rate or the number of respiratory cycles per minute, the patient is placed in the supine position, without the individual noticing that the observer's attention is directed to controlling the respiratory rate. The normal rate is 12-16 cycles per minute.
TEMPERATURE
Body temperature is controlled by the thermoregulatory center in the preoptic area of the hypothalamus. The normal temperature in the mouth can vary between 35.8 and 37.3 ° C and the axillary temperature up to 37 ° C. Rectal temperature is 0.5 ° higher than oral temperature. The method to determine it can be manual, with the back of the fingers on the forehead, or by means of a mercury, digital or electric thermometer, graduated from 35 to 42 ° C.
Methodology . The temperature can be measured in the patient's mouth, under the tongue, where the thermometer is placed for 3-5 minutes, with the mouth closed. The record is then read, and it is reinserted into the mouth for one more minute. If a variation is found between the two measurements, the procedure is repeated until the temperature stabilizes.
To measure rectal temperature, the thermometer at 35 ° C is inserted into the rectum, where it will be left for 3 minutes. This method is useful in infants and children. In these, the rectal temperature is higher than in adults, not lower than 37.2 ° C up to four years. It can reach 38 ° C after a day of activity. In the case of an infant, it is placed on the lap of the mother or the nurse and, separating the buttocks with one hand, the lubricated thermometer is inserted into the rectal cavity. The axillary temperature, commonly used, provides inaccurate data.
WEIGHT AND HEIGHT
The determination of weight and height, such as that of the body surface using tables, is used in the monitoring of some diseases and for the administration of certain drugs.
The ideal weight has a wide range, and is governed by cultural and aesthetic motivations. The extremes of it, cachexia and obesity, are associated with a greater number of diseases and complications.
HABIT
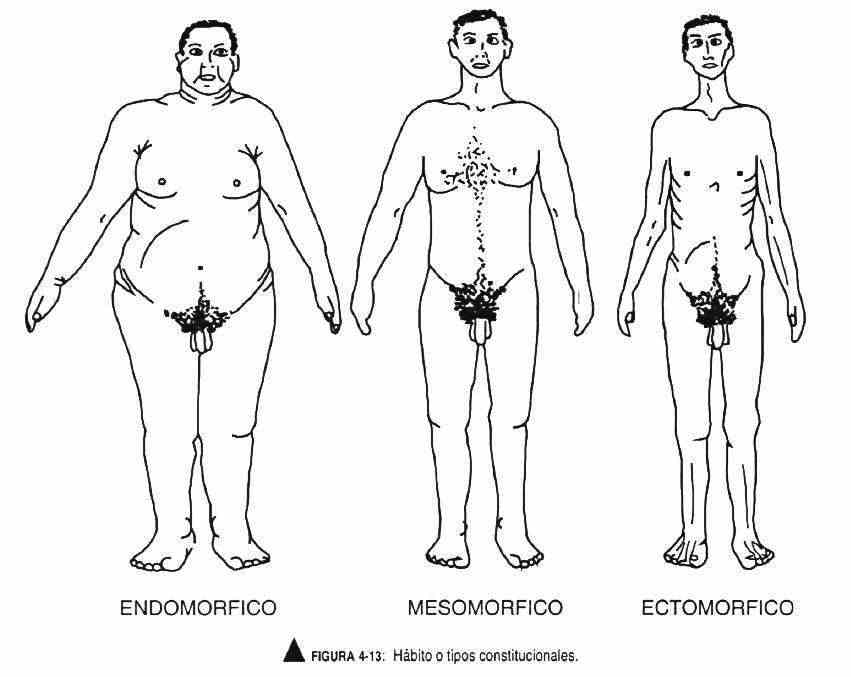
Habit is defined as the constitutional form or type or general proportions of the body.
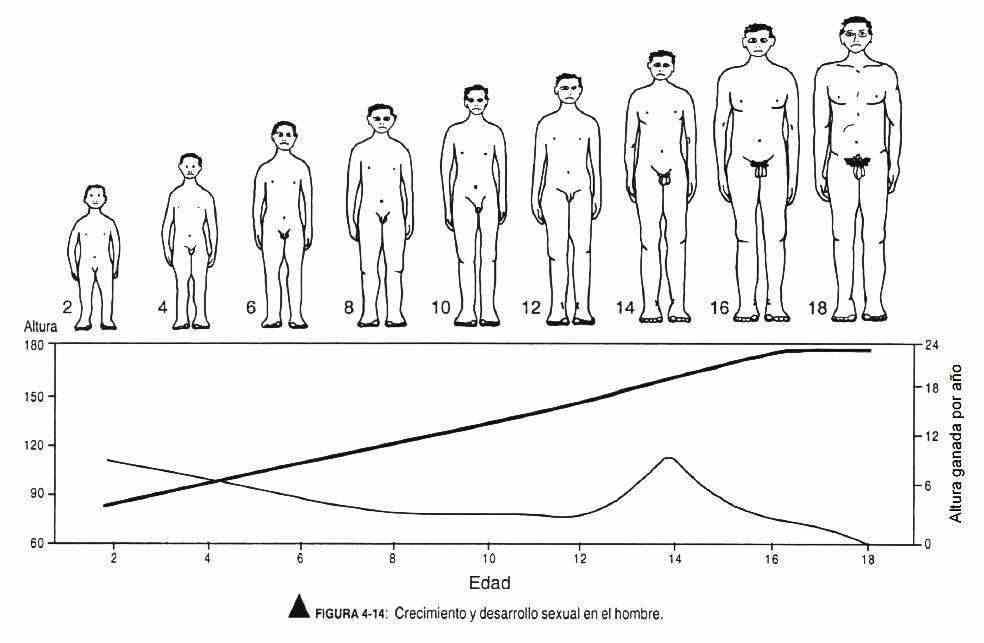
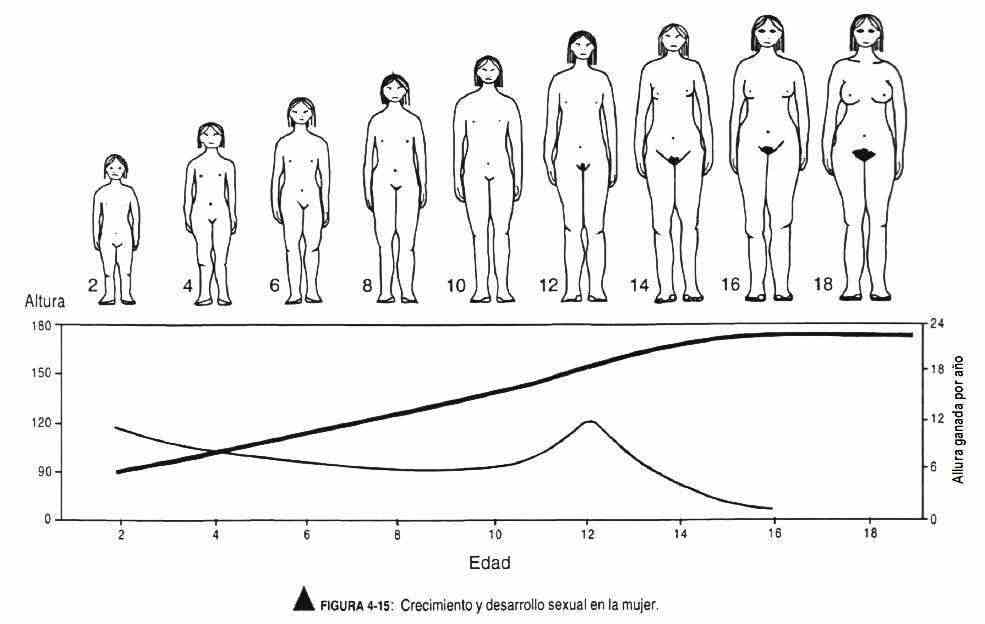
It is classically grouped into three body types (Figure 4-13). The asthenic-longilinear or ectomorphic type is thin, with elongated arms and legs, thin fingers, and a thorax with a reduced anteroposterior diameter. The picnic type has short arms and fingers, a protruding abdomen, a wide thorax and an adipose appearance, also called endomorphic. The muscular type, with a thick thorax neck, is solid in appearance and is called mesomorphic. Figures 4-14 and 4-15 correspond to diagrams of growth and sexual development in men and women.