by Alberto J. Muniagurria and Eduardo Baravalle
The neurological examination includes:
-
Motility test
- Examination of motility and strength
- Muscle tone test
- Trophism examination
- Presence of normal movements
- Test of muscle coordination or taxia
- Reflex test
- Sensitivity test
- Examination of the cranial nerves
- Study of the word and language
MOTILITY REVIEW
The striated musculature, innervated by the nervous system of relational life, executes voluntary movements. There are movements that do not depend on the will, which are associated movements and automatic movements, and reflex movements.
For a movement to be executed normally, with all the efficiency that this implies, it is necessary that an adequate contraction and relaxation of the agonist, synergist, fixative and antagonist muscles occur.
The examination of motility includes the study of the neuronal circuits of the pyramidal pathway, related to voluntary activity; of the extrapyramidal pathway, linked to attitude and posture; of reflections; and also of the cerebellum, which is the fundamental coordinator of movements and tone.
Examination of general motility and strength . To study general motility, the movements that the patient makes spontaneously when entering the office, when shaking hands, sitting down, speaking, taking off clothes, getting up from bed, walking, etc. will be observed.
In order to perform a thorough examination of the different muscle groups, the patient is given instructions to mobilize each muscle group. Thus, for example, you will be asked to tilt your neck forward, backward, on both sides, and look behind you, to assess flexion, extension, lateral bends, and rotations of the cervical spine. Successively all muscle groups will be evaluated, remembering the different movements that are carried out at each level.
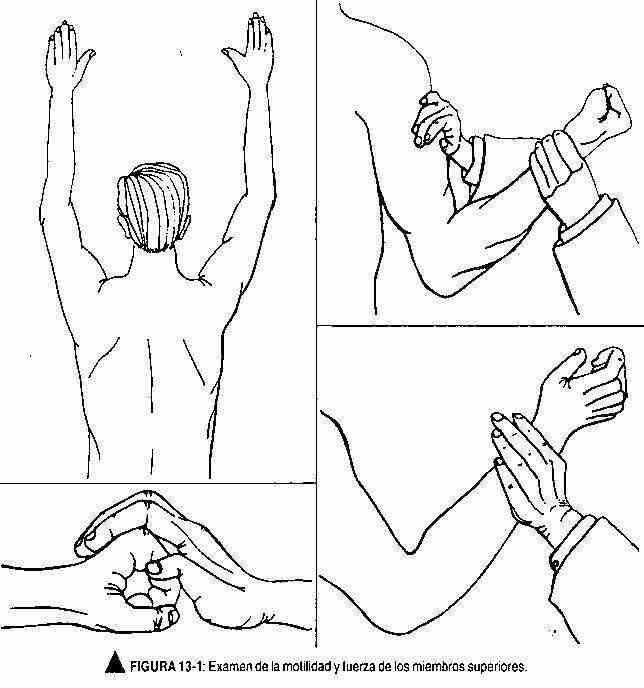
Once the movements have been examined, the strength of that movement should be evaluated, which can vary widely according to age, sex and the degree of muscle training. As this examination is carried out mainly by comparing the left side with the right side of the patient, the dominant hemisphere will also be taken into account or whether the right or left side of the patient is being inspected. This maneuver is performed by asking the patient to perform movements against an opposing resistance. Thus, for example, to assess flexion and extension of the upper limb, an attempt will be made to overcome flexion and subsequently an attempt will be made to flex the extended arm (Figure 13-1). A similar maneuver should be performed for each muscle group; for example,
When a decrease in motility and / or force is suspected that is concealed by the compensation provided by sight to maintain balance between the muscles, the patient should be asked to flex the upper limbs to 90 °, with the palms up, and close your eyes. The patient must be able to maintain this position (Figure 13-5). This same maneuver must be performed on the lower limbs; the patient, with eyes closed, in supine position, must be able to keep the hips flexed at 45 ° with the legs horizontal (figure 13-6), and in prone position they must be able to keep the knees bent (figure 13- 7).
Muscle tone test. Tone is the state of permanent semi-contraction exhibited by striated muscles, which gives them a particular consistency on palpation. It is produced by a monosynaptic and segmental reflex, which is the stretch reflex.
By palpation, muscle consistency is evaluated, which should be elastic in normal muscle. The patient is asked to relax or loosen, and the examiner grasps the patient's forearm with his left hand, and with his right hand flexes and extends the patient's wrist, assessing muscle tone. Similarly, it will do the same for flexion and extension of the elbow. These maneuvers will be repeated on the other side and a comparative evaluation will be performed. It will be carried out in the lower limbs evaluating the flexion of the knee and bringing the heel of the foot closer to the gluteal area; normally, the heel should not reach to touch it.
The states of nervous tension can produce alterations of the muscular tone; this is why the patient can be distracted by conversation.
Another maneuver may be used to assess muscle tone. With the patient relaxed, the examiner takes the patient's forearm, shakes it successively, and observes the movements of the hand.
Trophism examination. Muscle trophism depends on the peripheral motor neuron and circulatory status. The normality of the skin, hair and nails and the absence of trophic lesions will be inspected. In turn, the volume of the muscle masses and the normality of the joints should be evaluated.
With age it is possible to observe some loss of the muscular masses, and at the level of the hands there may be a slight atrophy of the thenar and hypothenar eminences and the most prominent tendons of the back of the hand can be observed.
Presence of abnormal movements. There is a physiological tremor of such small amplitude (10 oscillations / sec) that it goes unnoticed. It is detected by electrophysiological means.
Examination of muscle coordination or taxia. There are mechanisms that regulate motor coordination and that give harmony and regularity to movements. This coordination is regulated by deep sensation, the labyrinth, and the cerebellum. Sight also helps to maintain this balance.
There are various maneuvers to explore muscle coordination and gait.
The patient is asked to walk around the room, to come and go, observing the movements of the arms and legs and the associated rocking movements. He will then walk in a straight line with heel-toe or tandem gait (Figure 13-8, A).
Romberg test . With the patient standing, feet together and arms raised or close to the trunk, he is asked to close his eyes. Under normal conditions, the patient should be able to maintain balance and minimal oscillations can be observed. Minimal thrusts to the rear, to the front, or to the sides may occur and the patient must retain their position.
When examining a relatively healthy subject, he may be asked to alternately jump on each foot in the same place; the normality of this maneuver indicates intact motor function in the lower limbs, normal cerebellar function, and good positional sense (Figure 13-8, B).
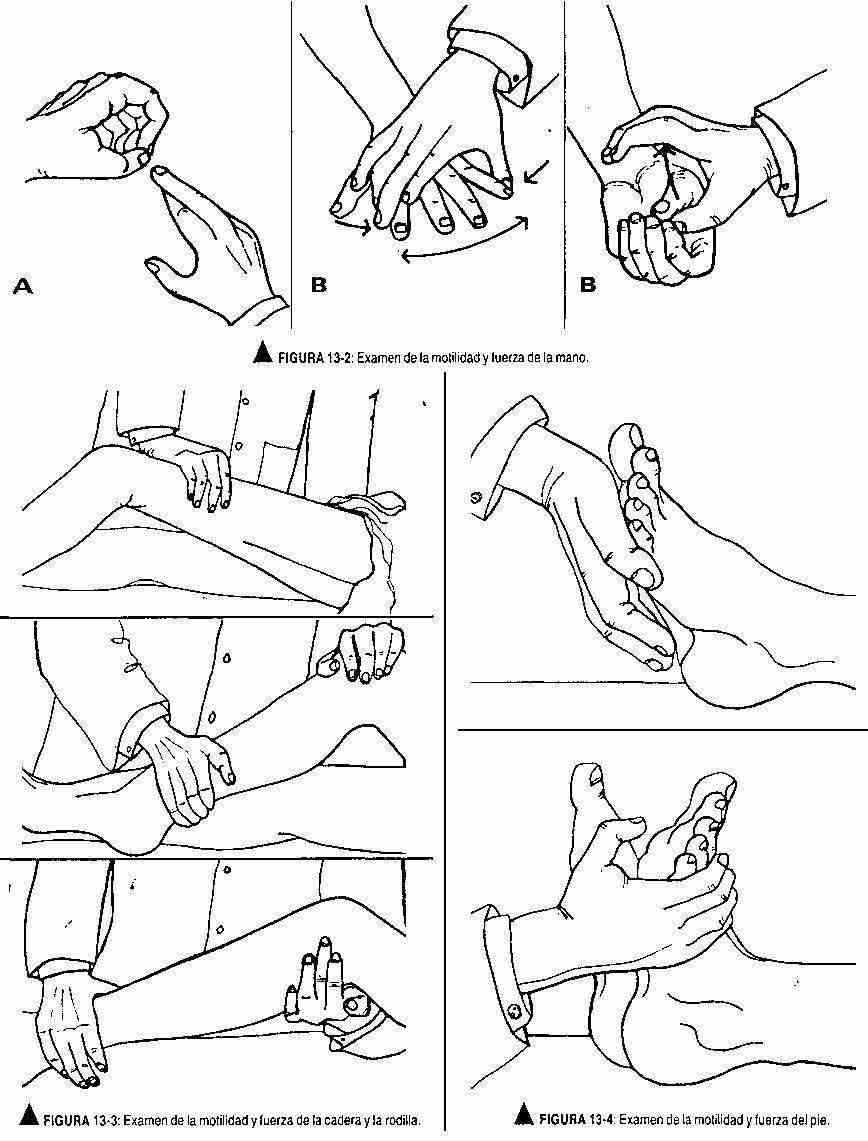
Arm coordination. The patient is asked to clap with the right hand on the left, alternately with the palm and the back. Later he will do the same maneuver, but in reverse. You are then asked to perform rapid pronation and supination movements with your arms extended. He is also asked to touch the tip of his nose and the tip of the observer's index finger with his index finger; This maneuver will also be carried out with the eyes closed. f The patient will be instructed to perform movements opposing the thumb with all fingers.
Coordination of the lower limbs. With the patient lying or sitting, the patient will be instructed to touch the left knee with the right heel, descend the anterior ridge of the tibia, and return the lower limb to its original position (Figure 13-9). This maneuver must be performed with both limbs and also, afterwards, with the eyes closed.
Reflex test. Reflexes are the simplest acts of the central nervous system and are, in turn, a fundamental manifestation.
The evaluation of the reflexes is carried out in both half bodies and a comparison is made between both sides. If the stimulus zone is a bone or tendon, the reflex will be osteotendinous, and if the stimulated area is the skin or mucosa, it will be called cutanemucosal.
To obtain a musculoskeletal reflex, the patient must be relaxed, with the limbs in the corresponding position for each reflex, and stimulate with the hammer quickly and directly in the reflex area.
The stimuli will not be very close to each other to prevent them from acting in the refractory period.
The hammer will be held with the hand, with the index and the thumb, to give the blow with more precision. The amplitude and rapidity of the response, and the relaxation should be evaluated. If there is difficulty in obtaining a reflex, it will be ruled out that this is due to the patient's nervous tension.
For this, there are distraction maneuvers, namely: 1) ask him about precise facts about his life or his family (dates of birth and / or ages), and 2) that he make an outward effort with hooked hands (figure 13- 10).
The answer can be 4+, 3+, 2+, 1+ and 0. A 4+ answer indicates a very fast and hyperactive reflex; generally indicates disease and is usually associated with clonus; 3+ is faster than normal and does not necessarily indicate disease; 2+ is normal; 1+ is decreased below normal and at 0 there is no response.
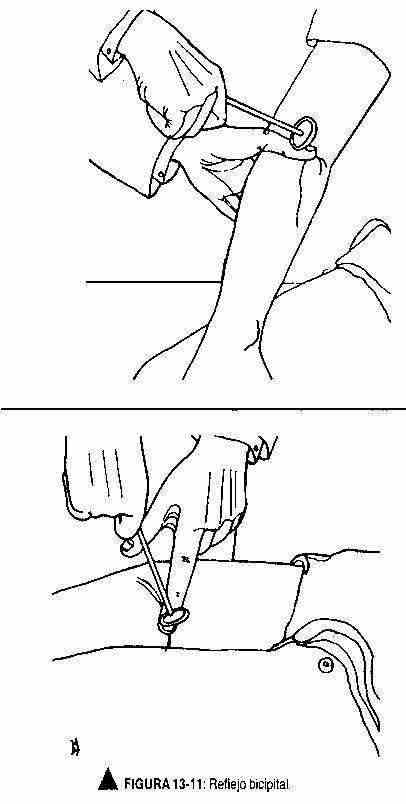
Osteotendinous reflexes. Bicipital reflex (C5-C6). The upper limb should be slightly flexed at the elbow, with the palmar surface down. The examiner will place his thumb or finger on the biceps tendon and stimulate that finger with the reflex hammer for forearm flexion, observing and feeling the contraction of the biceps (Figure 13-11).
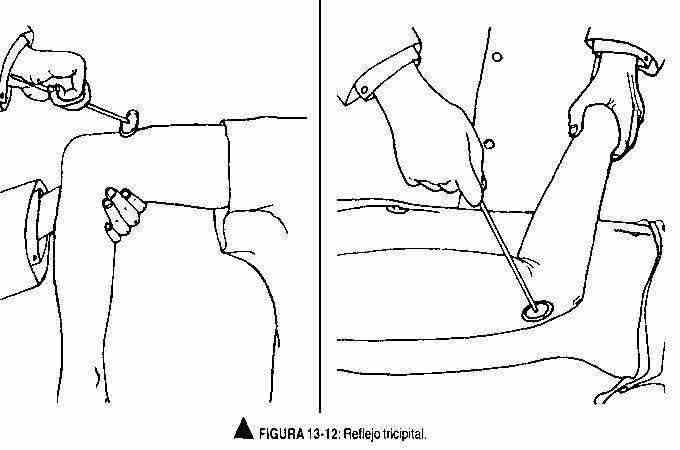
Tricipital reflex (C6-C7-C8). With the elbow flexed and palms down or resting gently on the chest, the triceps tendon is stimulated, above the elbow. Observe a contraction that produces elbow extension (Figure 13-12).
Supinator or brachioradial reflex (C5-C6). With the arm in the same position as for obtaining the bicipital reflex, or resting on the thigh with the palm facing down, the radius is stimulated, above the wrist. Note the flexion and supination of the forearm (Figure 13-13).
Cubitopronator reflex (C7-C8). With the arm in the same position as for obtaining the bicipital reflex, the ulna is stimulated above the wrist. The extension and pronation of the forearm should be observed.
Patellar reflex (L2-L3-L4). Also called the patellar reflex, it is obtained with the patient sitting or lying down; holding the knee from the popliteal fossa stimulates the patellar tendon. Note the quadriceps contraction with leg extension (Figure 13-14).
Achilles reflex (S1-S2). It is obtained with the leg flexed at the knee and dorsiflexed at the ankle, stimulating the Achilles tendon and observing the extension of the foot (Figure 13-15).
Cutaneous mucosal reflexes . The abdominal cutaneomucosos reflexes T8 to TIO above the navel and T10-T12 below it, are obtained by stimulating both sides of the navel, with a tongue depressor or needle, from the outside in, and observing the contraction of the abdominal muscles, which are manifested by the deviation of the umbilicus towards the stimulated side (Figure 13-16).
These reflexes are absent in the young child, since they appear at six months of life.
The plantar reflex (L4-L5-S1-S2) is obtained by stimulating the sole of the foot, with a key or a needle, following a line parallel to its outer edge, from the heel to the first toe. Flexion of all fingers should occur (Figure 13-17A). Dorsiflexion of the first toe and fanning of the rest of the fingers (Babinski's sign) are commonly seen in children up to the age of 2 years (Figure 13-17B). Its later presence is always pathological.
The abrupt stretch of the Achilles tendon obtained by a multiple and firm impulse against the plantar aspect of the forefoot, can produce small movements of flexion and extension of the foot of rapid extinction. When this response is not extinguished it is called clonus. It can also be obtained at the level of the patella by a sharp stretch of the quadriceps above the knee.
Stimulation of the chin area can produce a nuzzling or kissing motion. This response is normal in children, but acquires pathological value in adults. Manual stimulation of the palms of the hands may induce the stimulated hand to attempt to catch the explorer's hand. This reflex is called "grasping," and it has the same meaning as the sniffing reflex.
The cremaster reflex is obtained by stimulating the inner thigh by compression. Cremaster muscle contraction should occur, with elevation of the scrotum (Figure 13-16).
The bulbocavernosus reflex (S3-S4) is obtained by stimulating the skin of the glans with one hand, while with the other hand the contraction of the bulbocavernosus muscle is felt at the level of the bulbar portion of the urethra.
The corneal reflex is described by examination of the 5th cranial nerve.
SENSITIVITY TEST
In patients without neurological symptoms, an examination evaluating painful and vibratory sensitivity of the hands and feet, a comparative examination of the tactile sensitivity of the arms and legs, and a brief examination of stereoognosis will suffice. The detailed examination of sensitivity, which is fatigued to the patient and with which non-reproducible results are obtained, must be well planned and intended only for patients with nervous system symptoms or skin alterations.
A cotton swab, a pin, and an appropriate tuning fork are used for this examination. The patient will be given a proper explanation about the tests to be performed and will be asked to close their eyes. Symmetrical areas will be evaluated for comparison.
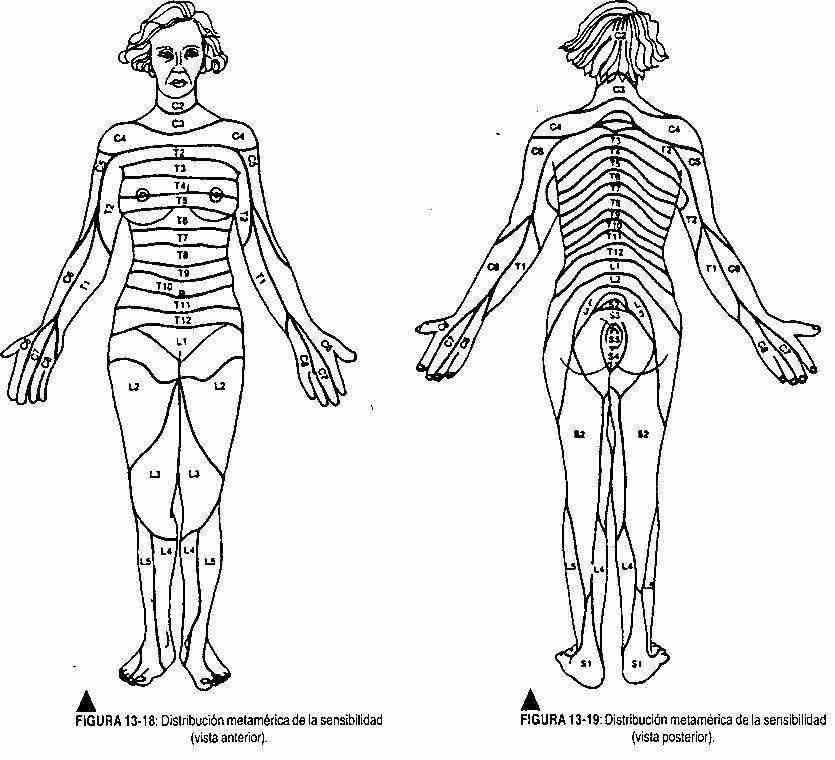
Examination of painful and tactile sensitivity. Alternatively, with the cotton swab and f with the pin, the different dermatomes (Figures 13-18 and 13-19) are examined from head to toe, and then a comparative evaluation is made between both hemibodies. The patient, with his eyes closed, must respond each time he is touched or pricked.
Examination of thermal sensitivity. With two tubes, one filled with hot water and the other with cold water, the different dermatomes are stimulated. This test is not performed routinely, but only when an alteration is suspected.
Vibration sensitivity test. The 256 Hz tuning fork is struck against the hand to put it into vibration and is supported by the areas to be explored: the bony prominences. Ask the patient what he feels; If you are not sure, you will be asked how far you feel vibrations and this will be controlled with the observer's fingers. It is usually performed on the bony extremities of the fingers and the malleoli.
Examination of positional sensitivity. Avoiding the contact of the big toe with its neighboring finger, the thumb and index fingers of the observer's hand mobilize the patient's big toe. You will be asked what position your finger is in.
Stereognosis test.An easily recognizable object (eg, coin, key, etc.) is placed in the patient's hand and asked to identify it. Likewise, numbers can be drawn on the patient's skin so that they can be recognized. He is also asked to discriminate between two nearby points when the fingertips are stimulated, trying to find the smallest possible distance in which he identifies the two points as different. Under normal conditions this distance is 2-3 mm. Furthermore, the patient must be able to point or locate with his finger the point where the stimulus has occurred. When two different sites are stimulated, you must be able to discriminate the stimulated sites. It can be said that the patient who performs these last three tests correctly has a normal sensory cortex.
It should be taken into account that with the use of needles and pins it is possible to transmit the hepatitis virus. Therefore, a history of liver disease or the appearance of blood with stimulation makes it necessary to discard the needles used.
EXAMINATION OF THE CRANIAL PAIRS
The examination of the cranial nerves, that is, of those nerves that innervate the structures of the head, is separated from that of the nerves that arise from the spinal cord. They can be systematically studied from par I to par XII.
Par I or olfactory nerve. The olfactory nerve examination is done through the ability to identify odors. Each nostril is evaluated separately with nonirritating substances such as coffee and tobacco. A nostril is occluded and with the eyes closed it is made to smell a certain aroma. Later the same test is carried out with the other nostril.
Par II or optic nerve. Examination of this nerve includes evaluation of visual acuity, visual field, fundus, and color vision.
Visual acuity. It is the means of evaluating the function of the macula. It is done in each eye separately, with different scales of letters of different sizes. The patient should be positioned 6 m from the graduated scales, and with one eye covered, should read the smallest line possible with the other. Visual acuity is expressed in a fraction, for example 20/30, where 20 is the distance at which the patient identifies the letters on the scale and 30 is the distance at which the normal eye sees it.
Visual fields. It is a method of evaluating peripheral vision. When a visual field alteration is suspected, a campimetry will be requested.
As a quick method, at the bedside of the patient, the patient and the doctor will sit facing each other, with the eyes at the same height and with a separation of 55 cm. The patient is asked to cover his right eye with his right hand while the doctor covers his left eye with his left hand. The right index finger of the examiner is placed in different places in the visual field. Every time the doctor sees it, it must also be seen by the patient (Figure 13-20). To evaluate the left eye, an identical maneuver is performed.
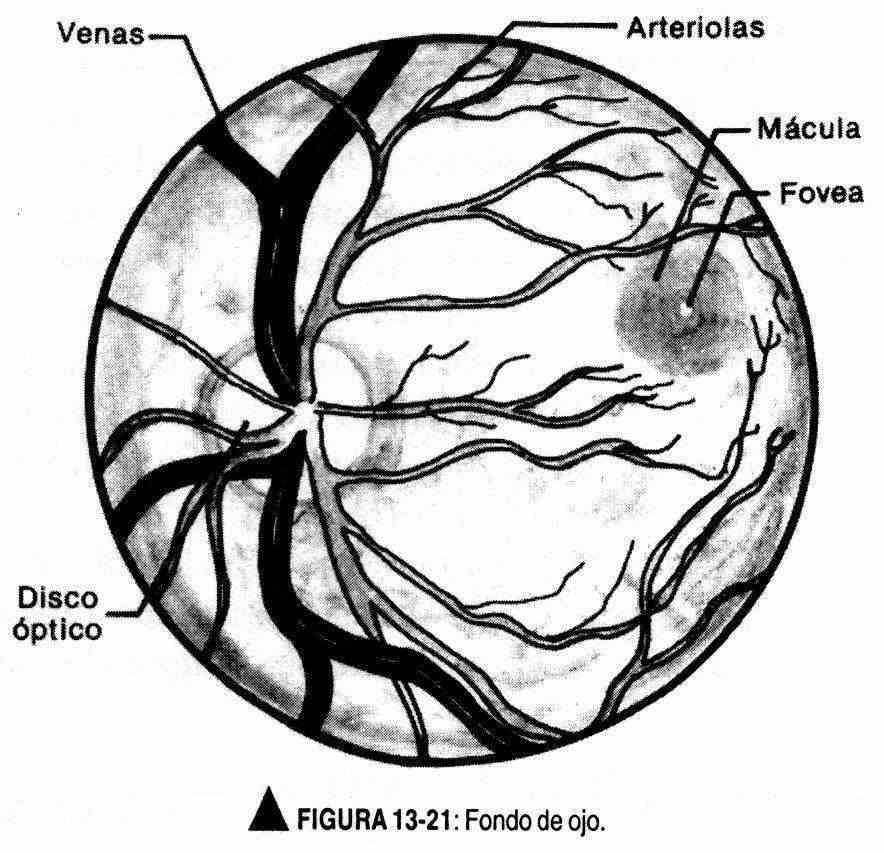
Eye fundus. The fundus inspection is performed with the ophthalmoscope, in a darkened room and usually with the patient's pupil unexpanded.
In special situations, when a more detailed examination is required, the pupil can be dilated with a mydriatic drug; the patient should look into the distance, trying not to move his eyes.
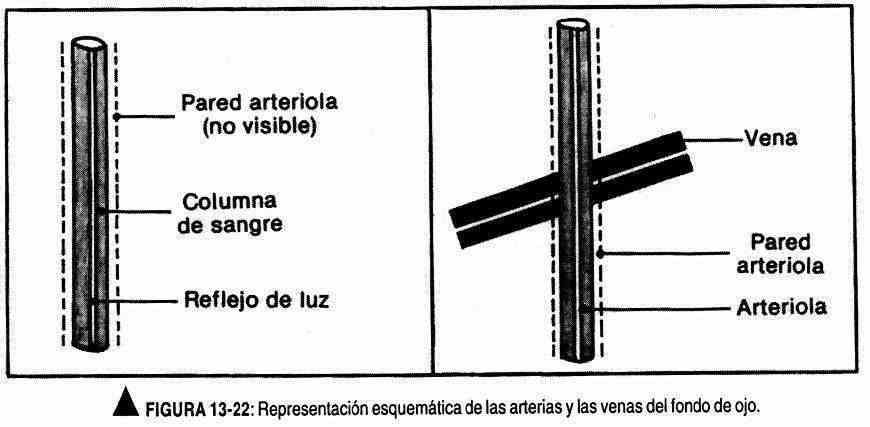
The right eye is examined with the ophthalmoscope in the right hand, and the left eye with the left hand. It is advisable for the patient to keep both eyes open; When beginning to look through the ophthalmoscope, the physician should be guided by the red reflex until good observation is achieved (Figure 13-21). To locate the disc of the papilla, follow the path of the vessels; As the veins approach the papilla, they increase in size. The disc appears as an oval or rounded structure, creamy-yellow in color. At this time, the ophthalmoscope diopters must be adjusted to clearly observe the structures of the fundus. Normally, the nasal border of the papilla may be obliterated; likewise, their edges may have whitish or brownish pigmentation. In the veins that emerge from the disc it is possible to observe pulsations. The arterioles and veins must be identified. The arterioles are bright red and smooth, two-thirds or three-quarters the diameter of the veins, and have a bright reflection in light. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. The arterioles and veins must be identified. The arterioles are bright red and smooth, two-thirds or three-quarters the diameter of the veins, and have a bright reflection in light. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. The arterioles and veins must be identified. The arterioles are bright red and smooth, two-thirds or three-quarters the diameter of the veins, and have a bright reflection in light. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. The arterioles are bright red and smooth, two-thirds or three-quarters the diameter of the veins, and have a bright reflection in light. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. The arterioles are bright red and smooth, two-thirds or three-quarters the diameter of the veins, and have a bright reflection in light. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. The veins are dark red in color and do not reflect light. The vessels must be followed on their way to the periphery to observe the arteriovenous junctions (Figure 13-22). The macula is difficult to see without dilating the pupil, and it appears as an avascular area larger than the papilla and two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. and it appears as an avascular area larger than the papilla and located two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye. and it appears as an avascular area larger than the papilla and located two discs away from the optic disc. If you want to evaluate the presence of opacities at the level of the lenses or the vitreous humor, the ophthalmoscope diopters should be changed to +10 or +12 to focus on the most anterior area of the eye.
Vision of the heats. It is carried out with a sample of wool of different shades, asking the patient to indicate the green, blue, red tones, and so on.
Pairs III, IV and VI (common ocular motor, pathetic and external ocular motor). To evaluate these oculomotor pairs, the size and shape of the pupils should be observed, and the photomotor reflex, the accommodation reflex, and the consensual reflex should be looked for. The movements of the eyeballs in all six planes will also be examined.
Regarding the pupils, its circular shape, its central location, its size (which varies from 2 to 5 mm) and its equality must be observed.
Response to light is investigated with the patient looking into the distance. With a light directed towards the stimulated eye, the constrictive response of the iris (photomotor reflex) and the same response in the other non-stimulated eye (consensual reflex) should be observed. The photomotor reflex occurs due to the pupillary response to light. The light beam, by stimulating the retina, travels through the optic nerve to the midbrain where it synapses with the nucleus of Edinger and Westphal or photomotor nucleus. From there, through the III pair or common ocular motor nerve, it reaches the muscles of the iris, causing the pupil to contract. By stimulating the right retina, the fibers from the nasal side of the retina are conveyed to the left optic chiasm, to the midbrain, having identical connections;
The accommodation reflex is sought with the patient looking into the distance, and asking him to look at the examiner's finger that is approaching up to 7-10 cm from the bridge of the nose. A pupillary contraction and convergence of the eyeballs caused by the oculomotor muscles should be observed. In the accommodation reflex, three movements occur: 1) pupillary contraction, 2) convergence, and 3) thickening of the lenses due to relaxation of the intrinsic muscles of the eye. This last movement is not seen. The sensory pathways of this reflex are similar to those of vision, ranging from the retina to the occipital cortex and from there to the midbrain, reaching the eyeball through the external ocular motor.
The photomotor nucleus is a parasympathetic nucleus. Sympathetic fibers originate at the cervical level and reach the eye through the pericarotid plexus that follows the internal carotid and its ocular branches. These sympathetic fibers cause the pupil to dilate and the upper eyelid to lift.
Examination of ocular motility is carried out by following the examiner's finger, without movement of the head, which moves horizontally, then vertically and then diagonally (to the right, to the right and up, to the right and down, left, left and up and left and down). The pendulum or conjugate movement of both eyes should be observed, paying attention to the appearance of incoordination or muscle fatigue. In the extreme lateral gaze, small jerks of nystagmus may appear, which quickly wear out. This phenomenon is normal.
Under normal conditions, the upper eyelid covers the iris, and in up-down movements the supracorneal sclera should not be observed.
The coordinated movement of the eyes is carried out by the joint action of six muscles: superior rectus, inferior rectus, external rectus, internal rectus, greater oblique and minor oblique. CN VI innervates the external rectum; the IV pair to the greater oblique; and all other extrinsic muscles are innervated by the sixth pair or common ocular motor. This nerve also innervates the levator upper eyelid and, as already mentioned, provides parasympathetic innervation to the pupil.
Pair V or trigeminal nerve. The 5th cranial nerve is a motor and sensory nerve. It innervates the chewing muscles, and gives sensitivity to the front two thirds of the tongue and the face. To study the motility of the chewing muscles, the patient is asked to close the mouth tightly and the temporal and masseter muscles are palpated.
The sensitive part is evaluated in the territory of its three branches: ophthalmic, upper jaw and lower jaw. Sensitivity to touch and pain are evaluated with a cotton swab and a pin, also carrying out a comparative evaluation between the two half-faces.
Horn reflex. They are obtained by stimulating the patient's cornea with a cotton swab. Obtain occlusion of the palpebral fissure. This reflex is carried by pairs V and VII, through the orbicularis oculi (Figure 13-23).
R masseteric eflejo. With the mouth ajar, strike the observer's index placed f on the patient's chin. Observe the occlusion of the mouth. This reflex is trigeminal-trigeminal.
Par VII or facial nerve. This motor nerve innervates the facial muscles, and also provides gustatory innervation to the anterior two thirds of the tongue through one of its branches, the chorda tympani.
The motility examination is performed by observing the contraction and symmetry of the occipitofrontal muscle, closing the eyes and trying to open them, showing the teeth, smiling, inflating the cheeks. The examiner should look for asymmetries and muscle weakness.
The sensory part is not usually explored, which is only carried out in certain situations.
Pair VIII or auditory nerve. The auditory nerve has two branches: the cochlear or auditory branch, and the vestibular branch in relation to balance.
Cochlear branch. In a rude way it is investigated with the ticking of the clock or with the noise of the nails or the rubbing of the fingers of the explorer. It is carried out first in one ear and then in the other. In case of certain anomalies, the patient will be instructed to perform an audiometry.
Lateralization test or Weber test. A vibrating tuning fork is placed in the middle of the forehead or at the interparietal suture, and the patient is asked where the vibrations are felt. In normal conditions the vibrations should not be lateralized; they should be felt in the middle or on both ears.
Comparison test between airway and bone conduction or Rinne's test. The vibrating tuning fork is placed on the mastoid process and, when the patient has stopped perceiving it, it is quickly placed near the ear. Under normal conditions, the airway conducts for longer than the bone route. The patient should hear the vibration in the ear after having stopped hearing it in the mastoid.
Vestibular branch. To explore the vestibular branch, the presence of spontaneous and provoked nystagmus, the Romberg test, and the static coordination tests (Rademaker tests) and dynamic (finger-nose) and gait tests are evaluated. Only nystagmus will be described in this section. The other tests are described in other sections.
Nystagmus is a oscillating, trembling, rhythmic, bilateral and symmetrical movement that can occur in extreme lateral gaze of the eyes. It has two phases of movement, one fast and the other slow, and of these it is the fast phase that gives it direction; for example, if the fast phase is to the right, the nystagmus will be a nystagmus to the right. Nystagmus can be seen in extreme vertical gaze or extreme horizontal gaze. This rhythmic movement can occur in a normal individual, but in this case it is very early extinction.
Nystagmus can be induced with rotary movements or by caloric or galvanic methods: It appears when a labyrinth is stimulated, with the fast phase directed towards the irritated labyrinth.
To study it with the rotary movement, the patient is placed in a chair that has a rotary movement, it is made to turn and it is stopped abruptly. In the normal subject, a nystagmus can be observed with its rapid phase directed in the opposite direction to the direction of rotation, which should be exhausted after 40 seconds. The lack of appearance of nystagmus is abnormal.
To obtain nystagmus by caloric methods, water at 44 ° C is introduced into the external auditory canal. Under normal conditions a nystagmus with its rapid phase towards the stimulated ear should be observed. With cold water (28 ° C) the nystagmus is directed towards the unstimulated side.
The galvanic test is performed by stimulating the mastoid processes with galvanic current, from 2 to 5 milliamps. A nystagmus directed toward the negative pole usually appears.
Abnormal nystagmus is a disorder of eye posture. It is caused by disease of the labyrinth, cerebellum, drug toxicity, or irritability of the cervical spine due to osteoarthritis. When both phases of nystagmus are the same, it is called pendulum nystagmus. There is also rotatory nystagmus.
Pairs IX and X (glossopharyngeal and vagus). The IX cranial nerve (glossopharyngeal) is a sensory and motor nerve. It carries the sensitivity and taste sense of the back of the tongue and the sensitivity of the oropharynx. In addition, it provides motility to the muscles of the oropharynx.
The patient should be asked to say "A" and observe how the soft palate rises, in a symmetrical movement; The sense of taste on the back of the tongue will also be evaluated. With a gentle touch at the level of the oropharynx, the gag reflex should be produced. The exploration of this cranial nerve includes the evaluation of the characteristics of the voice.
The X pair or vagus nerve innervates the pharynx and larynx, and carries parasympathetic innervation to the lungs, heart, and digestive tract.
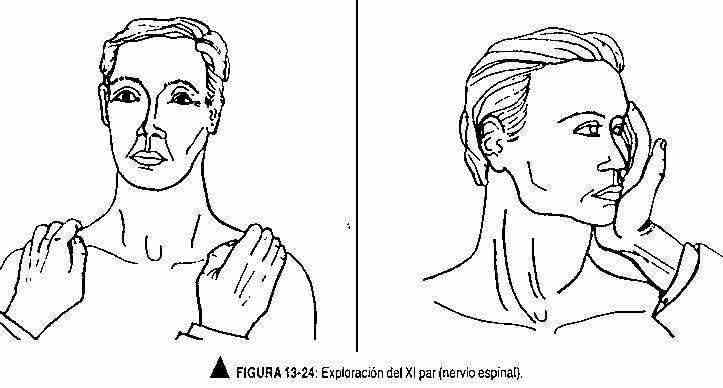
Pair XI or spinal. The spinal nerve is a motor nerve. It governs the motility of the trapezius and sternocleidomastoid muscles. Its exploration includes the evaluation of the trophic state of both muscles and the presence or absence of fasciculations at that level. The patient should be asked to lift the shoulders forward to explore the trapezius muscle. To examine the sternocleidomastoid muscle, the patient is asked to rotate the neck against resistance (Figure 13-24).
Par XII or hypoglossal. The hypoglossal nerve innervates the muscles of the tongue. The patient is asked to bring the tongue forward, up, and to the sides. In addition, he is asked to push the cheeks with the tip of the tongue, thus evaluating the strength of the tongue muscles; The presence or absence of fasciculations should also be noted.
STUDY OF THE WORD AND LANGUAGE
The study of speech and language are described in the section: "Studies of intellectual function", in the corresponding chapter.