by Alberto J. Muniagurria and Eduardo Baravalle
ALTERATIONS OF THE MENTAL STATE
General behavioral disturbances . The patient may present a face of anxiety, anguish, fear, depression, melancholy or anger. If all facial expressions are missing, think about Parkinson's disease. The euphoric attitude of the manic syndrome is typical, while flat affects and excitability and affective detachment characterize schizophrenia, which should not be confused with the slowness, dullness, indifference and lack of richness of thought that distinguish organic brain syndrome . Anger, hostility, and bombast are typical of the paranoid syndrome.
Conversation disturbances . The slow, boring conversation that tires the observer is the heritage of the hypothyroid, who also has a hoarse voice. It is also slow in depressive syndrome, and fast in manic syndrome. In the schizophrenic syndrome the conversation is intellectualized, complex and with neologisms. In the confusional syndrome it is disjointed, poor and meaningless. In the deaf it is performed with a higher vocal intensity.
Alterations of mood . The depressive syndrome is frequent in modern society, in which individual and social freedom are frequently affected. This syndrome, in its greatest form, is characterized by: 1) a feeling of feeling bad, sad, with a gray vision of the world and frequent crying episodes; 2) generally morning fatigue or asthenia; 3) sleep disorders; 4) inability to concentrate and decreased memory; 5) hypochondriacal thoughts, with frequent medical consultations; 6) appetite disorders; 7) decreased libido; 8) reduced language content, with poor ideation and suicidal thoughts.
Depressions can be secondary to a conflict situation (exogenous depression) or originate without apparent cause (endogenous depression). In addition, there are diseases that may begin or course at some point in their evolution with depressive symptoms, such as hypothyroidism, calcium and phosphorus disorders, pancreatic cancer, Parkinson's disease, rheumatoid arthritis, etc. Other times the patient has depressive symptoms that are part of a psychiatric illness such as dementia and schizophrenia.
On the other hand, if the patient has had manic behaviors and depressive symptoms in the last two years (shorter and less severe than a major depression), and without psychotic events, cyclothymia should be taken into account.
If depressive symptoms are less severe than in major depression and have been present in the past two years, or in the past year if the patient is an adolescent, and no psychotic symptoms have occurred, the likely diagnosis will be dysthymic disorder.
Alterations in the methodology and content of thought . It will be important to be able to detect some of the facts that are defined below. It should not be forgotten that language is the mirror of the mind. Generating anxiety in the patient, which can simulate organic alterations, should be avoided as much as possible.
- Circumstantiality. It is detailed thinking, in which the central idea can be lost, or if it is not lost, trivial facts are described in detail, interconnected, but without reaching the central point. It can be seen in normal or obsessive people.
- Loss of association of ideas. It is the leap from one idea to the other without any relationship between them and without the patient noticing. It can be seen in psychoses (manic, schizophrenia).
- Neologisms. They are made up words, which only have meaning for the patient, and are observed in certain psychoses.
- Flight of ideas. The patient jumps from one topic to another without a solution of continuity.
- Incoherence. It is meaningless thinking, either due to the presence of neologisms, or due to grammatical failures that make it unintelligible. It is observed in psychotics.
- Blockages It is the sudden interruption of thought in the middle of an idea or phrase. It occurs in normal people and in schizophrenia.
- Collusion. The absences or lack of memory in a story are filled by facts or events of the patient. It is seen in organic amnesic syndrome.
- Perseveration. The patient says what has already been said repeatedly. It is seen in dementias and psychosis.
- Echolalia The patient repeats the last word, syllable or phrase of others or his own. It is seen in dementias and psychosis.
- "Clanging". It is the choice of words for their sound. It is seen in dementias and psychosis.
The content of the thought can give an idea of the mental state and the state of mind, memory and the presence of compulsive ideas, anxiety, phobias, obsessions, delusions and associations of unreality.
Anxiety . It is a situation of doubt or insecurity that occurs irrationally. Anxiety is its peripheral expression and is manifested by sweating of the hands, palpitations, tachypnea, epigastric tightness and intestinal spasms. The patient may present with sustained anxiety and anguish, without apparent reasons or triggering by trigger objects.
Anxiety can be a response to a single stimulus (elevator, stairs) constituting phobias, or to multiple stimuli, and become an almost permanent manifestation of the individual. It can be evidenced acutely through panic attacks, when in the presence of the trigger object.
Compulsion . It is a behavior that is executed impulsively, that has no meaning or reason for being and that is carried out in order to avoid greater evils. Example: wearing braces and a belt at the same time for fear of pants falling off.
Obsessions . They are parasitic or irresistible ideas that tend to invade all consciousness, reducing voluntary activity to a minimum. Example: the subject who is constantly washing his body and hands, plagued by ideas of "dirt".
These three facts -anxiety, compulsions and obsessions- are observed in different neurotic pictures (agoraphobia, claustrophobia, simple phobias, etc., which can present with or without panic attacks), although they can also be part of psychotic and dementia pictures .
Feeling of unreality . The patient feels that the environment around him, the objects and everything that surrounds him is strange.
Depersonalization . It is the feeling of loss of identity and of the traits that previously characterized the patient.
Delusions . They are sick, illogical, false and foreign ideas to the patient's own culture.
These three phenomena -feeling of unreality, depersonalization and delusions- are the heritage of dementia and psychosis (schizophrenia and paranoia).
Perception disturbances . They are the illusions and hallucinations. The illusion is a false perception from real objects, while hallucination is a perception without a real object, without an objective visual, auditory, olfactory, gustatory or total stimulus that excites the senses. They should not be confused with the false perceptions that occur during or when sleeping. Hallucinations and illusions characteristically accompany psychoses, such as schizophrenia and paranoia, although they can be seen rarely in organic brain syndromes, such as dementia and delirium.
Orientation alterations . They occur when attention and memory are impaired, as in organic brain syndromes: dementia, delirium, and in some drug or drug poisonings.
Attention disturbances . They are closely linked to memory disorders. They are evaluated through the digit retention test. Attention disorders are seen in organic brain syndromes, in psychoneurotic states, such as anxiety, and in depressive syndromes, and do not allow a distinction to be drawn between organic and psychiatric syndromes.
Memory disorders . They can be evaluated, for example, through the history of the gaucho and that of the angelic child (see below). Recent memory is impaired in organic brain syndromes, such as delirium and dementia. As is clear to suppose, it is closely related to the capacity of attention, and therefore it is disturbed when there are attention disorders.
Language disorders . These are discussed later along with the methods of screening for dysphasias, dyspraxia, and parietal lobe syndrome. Not all patients are subjected to these tests, but those who are suspected of suffering from these disorders.
Alterations of intelligence . They are evaluated with the different intelligence tests (see below). It is decreased in advanced organic brain syndromes, but remains intact or slightly decreased in psychosis. The tests are used to differentiate a retarded adult from an insane adult.
Vocabulary is an excellent indicator of intellectual level. Psychiatric patients retain the validity of their vocabulary. The tests also serve to differentiate insane from retarded.
Characteristically, abstract thinking is altered in the schizophrenic, with absurd deductions. Judgment is distorted in both organic and psychotic brain syndromes.
Intellectual function tests
Intelligence is assessed by taking knowledge of information, vocabulary, abstract reasoning and judgment, thinking, memory, attention, written and spoken language, etc.
Vocabulary test . The patient should be questioned about the meaning of each of the following words:
- Health
- Reading
- Guitar
- Misuse
- Mulberry
- Frustrated
- Gelatinous
- Piscatorial
It is enough if the patient clearly expresses his knowledge of the word; no exact definition is needed. Three or fewer correct answers: below normal mean; 4-6 correct: normal; 7 to 8 correct: above normal.
There is a high correlation between vocabulary level and general intelligence. It decreases slightly with age. In patients with intellectual impairment (excluding dysphasia), this test usually provides a reliable index of prior intelligence.
100-7 test . The patient is asked to subtract 7 from 100, and then 7 from each result. The observer must ensure that he understood the test, and according to his own judgment may use any form of stimulus that gives the patient the real number. The patient's responses are recorded, as well as the time taken to perform the test. The ability to perform the test is sometimes impaired in cases of organic intellectual impairment (eg, Alzheimer's dementia) and also in psychoneurotic states. Despite this, this test does not allow discriminations between these two tables.
The Babcock judgment. "There is a necessary element for a nation to be rich and great: the safe and large supply of wood."
The phrase is repeated by the examiner and the patient, until the two are identical, or until eight attempts are made without success. The impairment is common in moderate organic diseases, including dysphasias and psychoneurotic disorders. Rude repetition of mistakes is typical of organic intellectual losses, while fragmentary repetitions suggest language defects. Coarse variations are characteristic of psychoneurotic pictures.
Similarities . The patient should be asked to explain the similarity between two words in the following pairs. Two points will be given for a good answer and one for a poor generalization.
| 2 points | 1 point | |
| 1. Dog and lion | both animals | they both have fur |
| 2. Eye and ear | sensory organs | both are part of the body |
| 3. Weighting-punishment | disciplinary methods | both affect one person |
Normal patients with low intellectual grade, or impaired, present great difficulties in this test. When the patient's responses mark differences and not similarities despite repeated explanations, the test suggests deterioration. A result of two points or less suggests impairment, especially if the vocabulary level is normal.
Digit retention . It is used to assess attention and memory (Table 32-1). The number of digits to be used in the first series is likely to be repeated correctly by the patient. Special care must be taken not to impart any kind of rhythm or stress. If the patient fails with a series of digits of a given number (619472), he must be tested with a series of the same number but from another column (392437). If the patient repeats the series of digits exactly, he will be tested with the subsequent larger series; if it fails in three consecutive attempts, it must be tested with a lower number, and so on until a number is reached in which the patient can, in three consecutive attempts, answer correctly.
|
Table 32-1 Digit Hold |
||||
| 582 | 694 | 641 | 352 | 837 |
| 6439 | 7286 | 4792 | 3852 | 7261 |
| 42731 | 75836 | 31859 | 48372 | 67183 |
| 619472 | 392437 | 472859 | 529746 | 728394 |
| 5917428 | 4179386 | 2183439 | 9278475 | 8129365 |
| 58192647 | 38295174 | 72594836 | 47153962 | 41935826 |
| 275862584 | 717942565 | 596138274 | 925841736 | 472916835 |
Other useful tests for the evaluation of thinking and intelligence are the following:
Explain the meaning of simple proverbs. Eg: "Bird in hand is better than a hundred flying."
Simple arithmetic calculations . If my watch costs $ 1.60, how many watches can I buy for $ 7.40.
General knowledge test
- The name of the current President, and that of his predecessors
- The name of the ministers
- The capitals of Italy, United States, France
- National dates
- The color of traffic lights
Memory . The patient is asked to repeat in his own words little stories that the examiner has read to him. For example:
- A gaucho arrived in Puerto Argentino with his dog, he left it at his friend's house while he bought new clothes. Dressed in his new suit, he went back to where his dog was, whistled at him, called him by name, and patted him. The dog did not recognize his master in his new attire, giving a pitiful howl. The caresses had no effect, so the gaucho put on his old clothes again and the dog immediately showed his joy again when he saw his master dressed as he thought he had to be.
- At the coronation of one of the Popes, three hundred years ago, a little boy was chosen to take part in the role of an angel; to make his appearance magnificent, they covered him from head to toe in a golden dress. The boy fell ill, and despite the fact that everything was done for his recovery, except to remove his gold dress, he died in a few hours.
Writing a letter. The patient is asked to write, within the next twenty-four hours, a report of his life.
EXAMINATION SCHEME FOR DYSPHASIAS, DYSPRAXIES AND PARIETAL LOBE DYSFUNCTION
Dysfasias
Aphasia, or to a lesser degree dysphasia, is a more or less exclusive loss of emission or understanding of language, spoken or written. It is due to a brain disorder. It must be differentiated from anarthria or dysarthria, which is produced by defects in the articulation of language as a consequence of muscular disorders, and from aphonia or dysphonia that is due to the loss of voice due to laryngeal defects.
Before beginning the examination, it is important for the examiner to ensure that the patient does not suffer from a confusional state, and if so, to what degree. Confusion will lead to difficult understanding and the formulation of verbal symbols that will give rise to the symptoms of dysphasia. Even the experienced observer may find it difficult to decide whether the degree of confusion is sufficient to produce the dysphasia that is detected.
To avoid as much as possible the effects of fatigue, the examination of the speech function in a patient suspected of suffering from dysphasia should be carried out in separate interviews, which should not exceed 15-20 minutes. The patient should be comfortable. The purposes of these interviews will be explained to the patient in appropriate terms. If there is any failure in your responses, it should be minimized with sympathy and encouragement. Every effort will be made so that you are not discouraged in tests in which you have been incompetent. The responses arising will be noted in detail, and will indicate which test may be of value in other investigations to be developed with the patient.
The simplest routine tests are as follows:
Ability to understand spoken words . The patient is given a series of verbal commands. First you should tell him: "Close your eyes", then "Take my hand."
If these requests are obeyed promptly and correctly, more complicated orders can be issued. Namely: "Touch your nose" and "Touch your left ear." If the answer to these indications is correct, the following will be: "Touch your right ear with the index finger of your left hand." If the exercise is done well, continue with: "When I put both hands in my pockets, but not before, hold on to my left hand." The examiner must be careful not to gesture the desired response.
Ability to understand written words . A series of written orders will be presented to the patient, successively and of increasing complexity. The indication must be legibly handwritten and if it is not interpreted by the patient, it must be repeated in block letters.
The orders are:
- Open your mouth
- Stick out your tongue
- Put your hand on the tie
- Aim for your left eye
- Touch your right ear with your left thumb
- When I raise my right hand above my head, and not before, take a pencil or other common object.
Ability to express themselves with speech . There is no formal test for this. It must be observed and transcribed. Note should be taken of grammatical and syntax defects, jargon use, and the ability to complete sentences, as well as possible word formation failures. The stimulus to speak should be appropriate for the patient and the circumstances, giving as an example: "How are you?", "Where do you live?", Or "Tell me about your accident", "I heard that you are interested in ... (work, hobby) "," I have been told that you like ... ".
The examiner should behave naturally during the conversation, using appropriate expression and gestures to elicit responses.
Ability to express themselves in writing . The patient is given a pencil and paper, and is asked to write a report of the weather, of his own sufferings, of recent news in the newspaper, or of important events in his life or previous occupation.
Ability to name objects . The patient is asked to name a series of common objects that are shown to him. Through this test, small levels of aphasia are revealed. It may happen that a patient is able to correctly name all the objects except one, and that this is as familiar as a pencil, even though he can describe it by differentiating it by its use, such as "it is used to write." Objects must be displayed in the following order (easily nameable ones interspersed with more difficult ones):
- Coin
- Button
- Handkerchief
- Pencil
- Wristwatch
- Pen
- Necklace
- Pack of cigarettes
- Blotting paper
- Pin
- Pair of twins
- Paper
- Toothbrush
- Lantern
- Ashtray
Reading aloud . The patient is asked to read aloud from a book or journal. A passage should be chosen that, beyond the defect produced by his dysphasia, is easy for the patient to understand. Any errors, misinterpretation and repetition of syllables will be noted.
Dispraxias
Apraxia consists of the difficulty or inability to perform acts with a correct sense, despite the fact that motor activity remains normal. Dyspraxia is a lesser degree of difficulty. In other words, there is an inability to perform muscle movements with a specific purpose, without there being muscle paralysis. As already mentioned in the case of dysphasia, also in dyspraxia it is important to rule out the presence of confusion and classify its degree. What has just been mentioned about the need for separate interviews, reassurance, and encouragement for the dysphasia examination also applies here.
History . Does the patient complain of inability to execute his habitual movements or his physical movements? Do you have difficulty shaving or dressing, or handling the knife and fork? Has a disability been brought to your attention? If so, is he aware of it? Is the disorder related to simple habitual movements or to acts that require more training? Does it affect a single member or all?
Orders supplied to the patient, who must comply.
Show me how you use:
- scissors
- Comb
-
the toothbrush
(The object is supplied to the patient in each case). - The patient is given a pack of cigarettes and a box of matches, asking him to light a cigarette.
- You are provided with a sheet and an envelope instructing you to fold the paper, and then close the envelope.
The following indications are given:
- Make a fist
- Applaud
- Scratch your head
- Stick out your tongue
- Close your eyes
- Stick out your tongue and scratch your head with your right hand
- Close your eyes and close your fist at the same time
- Wink
- Blow a kiss
- Greet
- Make "see you later" signs
- Pretend to close the door
- Pretend to count money
- Pretend to play the piano
- Simulate driving a car
The patient is given a number of matches, indicating that he builds figures imitating those built by the examiner on the table. In this way he is made to build a square, a triangle and a triangle above the square. When the results of these examinations are recorded, not only the failures should be noted, but also their nature and the patient's attitude towards the errors.
When studying dyspraxia, the following points should be kept in mind:
- The disorder may affect only one limb, or the entire body may be impaired in its ability to perform a desired movement.
- The patient may be able to perform a given movement spontaneously, but may fail to execute the movement in response to a command.
Failure to carry out a move can be caused by:
- Failure to understand the order, which constitutes sensory dysphasia.
- Orders that include the participation of manipulation, or use of objects that are not recognized by the patient (comprehension dysphasia). Perseverance can cause the patient to carry out movements appropriate to a previous command or in relation to previously displayed objects. Some degree of paralysis, sensory loss, or ataxia may be present. The patient's ability to imitate and respond to commands should be controlled.
Parietal lobe dysfunction
In patients with parietal lobe disease, a series of precautions should be taken to search for specific defects. Patients may have combined occipitoparietal, frontoparietal, and temporoparietal dysfunctions. These patients demand great attention from the examiner, both in collecting history and in investigative procedures. They are inconsistent, hypersuggestive, easily fatigued, scattered, sensitive, and easily changeable individuals. Furthermore, they rarely have an adequate understanding of the magnitude of their own shortcomings. If their flaws are openly shown to them during the interview, an emotional reaction may occur and the harmony between the patient and his examiner may be broken; therefore, the patient should be examined in a private and quiet environment,
All distractions that noise and noise can cause will be avoided. And the necessary efforts will be made not to draw attention to the mistakes that the patient makes during the studies.
Due to the inconsistency of the patient's responses to the indications, the same test, or type of test, must be repeated on different occasions and on different occasions. That is, if the patient fails to identify a common item, others should be shown, and then the unrecognized one should be included again, and so on.
It may happen that the patient who fails one opportunity does not do so the next, and then fails again. All these paradoxical responses must be faithfully noted.
To secure and maintain patient care, the examiner must be firm and unflappable.
The patient's care, once awakened, is not easily disengaged to proceed to the next problem. Due to the fatigue of the patient, the sessions should be short.
Therefore, repetition of the tests is necessary. Of great importance from the point of view of scientific evaluation is self-discipline in terms of firmness on the part of the examiner.
The doctor in charge of the case must record faithfully and in detail what the patient does and what he says, instead of interpreting what he assumes the test indicates. Therefore, if a patient recognizes an object that he is asked to identify (eg, a toothbrush), it will not be correct to write "the patient does not have objective agnosia." The correct way will be:
Question: What is this? (a toothbrush is shown).
Answers: "...... Let me see ...... I can't see it well ........ (The patient looks at the object, does it intensely, turning his head from side to side). .... It's a fork .... No ....... It's more like a pencil ....... Or not ...... I know ...... I think it is what you use to clean your teeth ........ That's ....... a toothbrush ........ (55 sec.). Or even "Object identification: toothbrush "(one minute).
In these cases, it is particularly misleading to use questionnaires or printed stories where rating ability is marked with a check mark or with a (+) or (-).
During these procedures it is useful to have a stopwatch to measure the time it takes the patient to perform the tests successfully.
A patient with parietal disease often reaches the correct conclusion only by chance, but the manner of doing so may be completely abnormal. The folder must include any indication of doubt, excitement, change of idea, surprise, or any interjection; Notes should include anything the examiner uses to stimulate the patient, as well as repetitions and questions. In this sense, a vivid, trustworthy and positive writing must be carried out so that a future reader is able to interpret how the patient behaved during the interview.
Sensory evaluation . Once again, in this case, the easy fatigue and inconsistency of the patient will be taken into account, and therefore the sessions should be short, quiet and frequently repeated. The examiner must be careful in observing any evidence of stresses occurring in the course of the tests. They can occur spontaneously, but are more frequent after the procedures used (tactile perseverations: palihaptia, diplohaptia and polyestesia).
The usual sensory modalities are explored, such as superficial touch (pen or cotton swab), pain (pin, rather than a needle), and particularly postural sensitivity.
The vibratory sensation should be evaluated with a tuning fork of 128-256 cycles.
Of great importance is the technique of double simultaneous control (with tactile and pain sensitivity). This maneuver can demonstrate tactile inattention (formally called extinction) which is an important sign of parietal disease. Bilateral contacts must be absolutely simultaneous, since even a short interval between the two stimuli can draw attention to their dual nature. After repeated monitoring, tactile inattention may "break down" and the patient proclaim, hesitating at first, "I think it is touching me on both hands."
The topognosis or location of the touch is also important. The patient, with his eyelids closed, must indicate the exact point where he is stimulated. The longer the stimulus is applied and the firmer the impact, the safer the localization is going to be. The most significant feature is the difference or variation in location security between the two stimulated areas. Sometimes the error in localization is extreme and the patient may even make the opposite projection error (alloesthesia or alloquiria), or vaguely point out some region in space (exosomatoestesia).
The tests for the tactile identification of objects on the palms of the hands are the most revealing (stereognosia). A wide variety of common objects can be used, varying their size and ignoring those that are not familiar. The examiner must observe how quickly the object is identified, and any difference between the two hands can be significant for astereognosia. Hence the value of a stopwatch. Similar objects, eg, two oranges, can be placed simultaneously on both hands, and the patient's responses should be noted. It will be observed which hand moves first to feel the object and which hand identifies it faster. The patient can recognize the orange placed in a hand, but can announce only after an interval " In patients with parietal disease, the orange on the affected hand will be felt as larger and heavier (macrostereognosis), and less frequently as smaller (microstereognosis). Here a factor of alteration or confusion intervenes. When the temperature difference between the palm of the hand and the object is significant, there is a tendency for the object to appear larger. Sometimes the patient correctly recognizes the object, but continues to misjudge the object's contours (metamorphotaxis). In patients with parietal disease, the orange on the affected hand will be felt as larger and heavier (macrostereognosis), and less frequently as smaller (microstereognosis). Here a factor of alteration or confusion intervenes. When the temperature difference between the palm of the hand and the object is significant, there is a tendency for the object to appear larger. Sometimes the patient correctly recognizes the object, but continues to misjudge the object's contours (metamorphotaxis). there is a tendency for the object to appear larger. Sometimes the patient correctly recognizes the object, but continues to misjudge the object's contours (metamorphotaxis). there is a tendency for the object to appear larger. Sometimes the patient correctly recognizes the object, but continues to misjudge the object's contours (metamorphotaxis).
In patients who have obtained a normal score on tests for stereognosia, a significant difference in skill between the two hands is sometimes demonstrated by asking them to identify common objects while wearing light cotton gloves. With this disadvantage, a latent unimanual astereognosia can be demonstrated.
In cases of dominant parietal lobe disease, special procedures must be used to demonstrate bilateral ideomotor apraxia. In these circumstances, the patient will be unable to execute complicated movements: clap, take a cork from a bottle; he will be clumsy in handling objects and unable to take out a match and light a cigarette or fold a letter and put it in an envelope. On a more "automatic" level, it can be objectively manifested that the patient has had difficulty using a fork, knife, dressing, or shaving.
Drawing of common places not in sight . In this section, drawing themes of an articulated feature will be chosen for the patient, such as a watch face, a flower, a bicycle. Sometimes spatial disturbances are shown when they try to draw a house, an airplane, a human figure. In these spontaneous drawings the presence of confusion of planes, alterations in perspective, dysfunction of the parts of the components and lack of completion of the symmetrical objects is sought.
Drawing maps . The patient is invited to draw for himself the map of the country where he lives, and to include six or seven cities of his own choice.
Drawing of plans . The patient draws a two-dimensional plan of a topographic site well known to him and the examiner. A person from Rosario may be asked to draw a plan of Parque Independencia. We can also tell you to draw a plan of your living room, with the doors, windows and furniture.
The examiner must be familiar with the current status of these tests so that he is not mistaken by conspiracy on the part of the patient. In the hospital setting, you may be asked to draw a map of the guard in which you were admitted and to mark the location of your own bed, bathrooms, and neighboring rooms.
To study spatial orientation, the patient can also be invited to draw a series of arrows directed to a given point, up to the right, down and to the left;
The patient with parietal disease can not only misalign the linear dimensions, but can also get lost with the obliqueness of the short lines that form the hairs of a bird feather.
The understanding of spatial notions expressed verbally should be checked by placing the patient in front of a table and ordering him to put his hand on or under the table, to stand in front, behind, to the left or to the right of it.
The patient is given a few pieces of wood that have been cut into different geometric shapes and that fit around their edges, and the patient should join them properly. This test has the additional merit of sometimes demonstrating video-spatial ignorance in one hemisphere. Common puzzles are an exercise in spatial manipulation that is far from the capacity of many parietal patients. A simple test can be done by taking a colored figure from a book, cutting it into four or six pieces, and inviting him to put the figure back together.
Using play dough or clay can also reveal results similar to 1; drawing drawings. The patient is given a quantity of one of these materials, of various colors, and he is invited to make simple shapes, such as a cup, a plate, a human head, a dog, a kettle, a giraffe.
To carry out this task, which may be totally unusual for him, he must be allowed complete privacy, and control the time it takes to carry it out. The forms made can be photographed to serve as permanent evidence. In some cases I work them; they may appear grotesque, being disproportionate, uneven, elongated, or truncated.
Construction apraxia tests
The examiner makes a drawing - simple or elaborate, or a minor squiggle asking the patient to copy it. Here only the copy ability is evaluated and not the elaboration capacity. In patients with constructive apraxia the ability to carry out this simple task is impaired, usually to extreme degrees.
A variant of the previous test consists of using, instead of paper and pencil, a series of matches. The examiner makes a design and the patient with his matches must copy the drawing.
More difficulty is added to the test if the Goldstein toothpicks, which consist of four-gauge toothpicks, are used. Once the examiner has made his drawing, the patient will make the copy.
Another demonstrative way to assess constructional apraxia in female patients is to allow them to enter the hospital kitchen, and to lay out a table for a meal for four. The patient should be left alone to do her homework, and she should be allowed access to all she wants of crockery and cutlery. Time is noted, and you can photograph how you have laid the table.
The tests with the Kohs blocks have a particular value in the evaluation of the parietal patient, but it must be taken into account that this technique is more complex than a mere evaluation test for constructional apraxia. Letters or blocks are used, each one with a part of a whole that when joined can form defined geometric figures. It is not necessary to use all the cards, but just use three or four. During the development of this test, a parietal patient, whether with a right or left lesion, will frequently show their impairment. In the first instance, he will usually show resistance or reluctance to embark on this test. The patient will do it slowly and reluctantly, taking the blocks one by one, as if to reveal their colors by showing the face up. Although only four blocks are needed, the patient will often start by choosing many or few. Another common flaw is that you can start to place one of the blocks on top of the pattern itself. From then on he will show the usual doubts; slowness and need to be corrected.
The patient will choose a block, turn it over, and, holding it slowly and carefully, return it to position, sometimes in an altered form. Throughout these maneuvers, the patient frequently appears confused and distressed. When the patient has finished his task, he can be satisfied, although there is little correlation with the proposed model. Less often the patient cannot express any opinion about the realization of the pattern.
Mistakes in your homework may be obvious. The blocks can form an open square instead of a closed one, or they can be offline. The geometric pattern of the form card may be completely different and not even related to colors.
Construction defects can be demonstrable in the patient's writing. The lines may not be built horizontally, or they may be directed up or down, and may even intersect. The left margin may be too wide, raising the suspicion of a missed left space lesion. The patient may be unable to put the hands in order.
Tests for body location (body image)
These tests are often imperfectly performed in patients with a predominantly right parietal lesion.
If the patient is observed at the time of dressing, numerous difficulties can be detected, many of them evidenced unilaterally. In other words, the patient can put on a stocking and a single slipper, or he can also forget about the sleeve on the right side when dressing. The term apraxia of dressing is used frequently, but it is preferable not to use such a definitive expression, but called, for example: "inability to dress".
The integrity of the body location can be evidenced by instructing the patient to touch different parts of their anatomy. The inability to perform this maneuver is called autotopognosia. Perhaps a special type of this difficulty is that known as finger agnosia.
There are several techniques to demonstrate it. For example: the patient will be instructed to show a particular finger, or the examiner may take a finger and ask what it is called.
Also the patient can touch or name fingers on the examiner's hand, and finally, the patient can touch or name fingers on a glove.
The right and left orientation requires special study. The patient will be instructed to quickly indicate either his right hand or his left hand, repeatedly and successively, noting the promptness and confidence of the response. The test can be continued by asking the patient to indicate the examiner's right or left arm. To increase the difficulty of the test, the examiner may cross his arms or legs. The test can be extended to inanimate objects: dolls, gloves, pair of shoes, etc. The patient's task should be accomplished as quickly as possible, both on the right and on the left.
Special attention should be paid to the existence of agnosia at the level of the fingers with right-left confusion, dyscalculia or dysgraphia. This constitutes the so-called Gersmann syndrome, which is the clinical expression of a lesion in the supramarginal gyrus of the dominant hemisphere.
Less well known is Leonhard's syndrome, which includes dyscalculia, dysgraphia, apraxia of construction, and temporal disorientation.
ABNORMAL FINDINGS ON THE EXPLORATION OF THE GAIT
Gait inspection can provide information on coordination and balance, the presence of muscle, joint, bone, and neurologic abnormalities, and the presence or absence of pain. The alterations can appear when the individual closes the eyes, and attention should be paid to the firmness of the gait, the amplitude of the base of support and the existence of associated movements.
Different types of gait are described, which by their characteristics define certain pathologies.
March of spastic hemiplegia . It is produced by injury to the cerebral motor neurons, with involvement on the side opposite to the injury, consisting of a flaccid paralysis that later becomes spastic, with moderate atrophy.
This gait is characterized by the fact that the patient has the affected upper limb in flexion, with the elbow, wrist, metacarpophalangeal and interphalangeal joints flexed. The affected lower limb is in extension and supports only the forefoot. During the movement, the patient first propels the foot outward to advance it, describing a circular or scythe motion.
March of the cerebellar syndrome . It is produced by injury to the brain or its pathways.
This gait resembles the gait of the drunkard, with increased base of support, inability to follow a straight line, and open arms in an attempt to help each other; It is an insecure, unstable, shaky gait, with difficulties in turning, which with eyes closed continues in the same way.
March of the sensory ataxic . This type of gait occurs in patients with absence of Castle's intrinsic factor, which causes disorders in the absorption of vitamin B12. There is degeneration of the posterior cords of the medulla or bundles of Goll and Burdach. This gait also appears due to direct injury at that level, with loss of deep sensation, and also in the tabes dorsalis.
It is characterized as an unsteady gait, in which the feet are placed with open legs, and the foot is thrown forward and out, striking the heel and forefoot first in an attempt to find the ground. The patient tends to balance with the arms. When he closes his eyes, he falls. These patients have a positive Romberg's sign.
March of the spastic in scissors . It is produced by spastic paresis of the lower limbs. This gait resembles the movements of a scissors; the thighs are propelled with greater force than necessary, giving the gait a characteristic rocking rhythm, with dragging of the toe. It resembles the march that is performed under water.
Parkinsonian gait . It is produced by degeneration of the nuclei of the base. The patient is propelled forward, with flexed hips and knees, and flexed, trembling, and akinetic arms. He has difficulty starting movements (he appears magnetized to the floor) and when he starts walking, he does so abruptly.
He also has difficulty stopping; it is a march of small steps. When the latter is the only characteristic it presents, it accompanies organic brain syndromes.
Steppage . It is produced by injury to the lower motor neuron or by paralysis of the external popliteal sciatic, and therefore of the lateral peroneal muscles.
This gait (Figure 32-1) is characterized by a dropped foot, and therefore the patient must flex the knee further to prevent the toes from hitting the ground. It is impossible for him to walk on his heels.
Myopathic gait . It is produced by injury to the muscles or by congenital hip dislocation. The patient walks with wobbling movements due to weakness of the pelvic girdle muscles.
Labyrinthine gait . It is a consequence of a labyrinth injury.
It is an unsafe, unstable gait, falling to the ground when the individual closes his eyes. If the patient walks back and forth with his eyes covered he describes a star, known as the Babinski star gait.
Trendelenburg march . It is caused by weakness of the abductor muscles of the thigh, due to muscle injury or nerve injury, or hip injury. It is characterized by a fall of the pelvis during gait rather than normal advancement on the side opposite the injury; in other words, when it supports the diseased side, the healthy hemipelvis descends.
March of the lame or the lame . It is caused by pain or shortening of a limb. It is characterized by a short gait on the side where the injury is located, with sinking on the diseased side and propelling the healthy side forward; the advance is greater on the healthy side.
March of Korea . It is observed in the disordered, elastic chorea, with many movements; the individual appears to fall, but is always saved from the fall.
ABNORMAL FINDINGS ON EXPLORATION OF THE CRANIAL PAIRS
Par I or olfactory nerve
They can be quantitative or qualitative, or consist of hallucinations and olfactory illusions.
Anosmia . It consists of the lack or loss of the sense of smell, usually bilateral; consultation for unilateral anosmia is rare. It is produced by injury to the mucosa or by hyperemia of it caused by different causes: acute or chronic inflammations of bacterial or viral, allergic, toxic (tobacco) or hormonal origin, which block the access of volatile particles towards the receptor. There is a picture of congenital anosmia due to a defect in the hypothalamic area and with gonadotrophic hypogonadism, known as Kallman syndrome.
Anosmias can also be of traumatic origin (ethmoid fractures), neoplastic (meningiomas of the frontal area, pituitary tumors, craniopharyngiomas, frontal tumors) or due to arterial malformations (aneurysms of the anterior portion of the polygon of Willis). Foster-Kennedy syndrome includes anosmia and atrophy of the optic nerve due to frontal lobe tumor. Unilateral anosmias are usually neoplastic or traumatic in origin.
Hyposmia . It is the decrease in smell. It is usually produced by injury to the receptor.
Hyperosmia . This is the name given to the increase in olfactory sensations. It can be seen in hyperemesis gravidarum and cocaine intoxication. These pictures must be differentiated from hysterical hyperosmia.
Parosmia or dysosmia . They are subjective alterations of the sense of smell. They can be seen during recovery from anosmias. They are characterized by the sensation of bad smell (cacosmia) and are accompanied by alterations in taste.
Olfactory illusions and hallucinations . They are seen frequently in schizophrenic psychosis; they occasionally accompany alcohol withdrawal syndromes and uncus seizures. Small parosmias are not always related to psychiatric illnesses. They can appear and disappear according to different stimuli (phantosmia).
Par II or optic nerve
 Visual acuity disturbances.
Visual acuity disturbances.
Refraction disorders . Myopia. It is the refractive disorder in which the image is formed in front of the retina (Figure 32-2, A), due to a lengthening of the anteroposterior axis of the eye. In other words, the nearsighted person does not see from afar but up close, even small details can be seen well.
Hyperopia . It is the refractive disorder in which the image is formed behind the retina due to a shortening of the anteroposterior axis of the eye (Figure 32-2, B).
This means that the hyperopic person does not see up close, but sees correctly from far away. In presbyopia the visual disorder is the same, although caused by a decrease in the elasticity of the lens.
Astigmatism . It is the refractive disorder in which the different corneal diameters have uneven curvatures, focusing on different points.
Asthenopia . Asthenopia or visual fatigue can be due to accommodation or muscle disorders. Accommodative asthenopia can appear in hyperopic or astigmatic individuals, who must accommodate their sight for long periods of time, or in asthenic, cachectic individuals, who cannot maintain the effort of accommodation. Muscle asthenopia is seen in myopic patients, due to muscle exhaustion of the internal rectus muscles to see closely. These muscles cannot maintain convergence.
Media disorders . Clarity of the media is essential for correct viewing.
The cornea can become cloudy, leading to poor vision. Keratitis or corneal opacification can occur in hereditary syphilis or after herpes infections (simplex or zoster) and in association with uveitis and iritis in Behget's disease and Reiter's disease; with skin lesions in Stevens-Johnson syndrome, and with post-traumatic lesions or walleye. In some of the mucopolysaccharidoses (eg, Hurler's) polysaccharides accumulate in the form of clouds, sometimes depositing on the refractive media. Band keratitis is caused by calcium carbonate and phosphate deposits in the corneal epithelium in all diseases associated with hypercalcemia.
Other times, a green or yellow gold ring is observed due to copper deposition in the corneal epithelium. This ring is called the Kayser-Fleisher ring and is seen in hepatolenticular degeneration or Wilson's disease, which can also be accompanied by cataracts. It is also possible to observe it in primary biliary cirrhosis.
In addition, the senile arch can be found in the cornea, which is observed on the periphery of the cornea, is bluish-white in color and is seen in elderly, hyperlipidemic and alcoholic individuals; does not cause vision disturbances. Cistern crystals can also be deposited in cysteinosis, and chloroquine and amiodarone crystals can be deposited during treatments with these drugs.
 The aqueous humor can present an increase in its intraocular pressure (normal, up to 15 mmHg) giving rise to glaucoma. There are open-angle (angle between the iris and the cornea), closed-angle and congenital glaucomas.
The aqueous humor can present an increase in its intraocular pressure (normal, up to 15 mmHg) giving rise to glaucoma. There are open-angle (angle between the iris and the cornea), closed-angle and congenital glaucomas.
Congenital glaucoma frequently accompanies other congenital anomalies such as aniridia, microcornea, spherophakia, primary persistent hyperplastic vitreous, SturgeWeber syndrome (ataxia-telangiectasia), von Recklinghausen neurofibromatosis (café au lait macules, and neurofibromas), Marfan syndrome, Pierre Robin syndrome (micrognathia and glossoptosis), homocystinuria, and congenital rubella.
Glaucoma is open-angle in 90% of cases, and in them the cause of the lack of aqueous humor drainage is unknown. 5% is closed-angle and is due to the use of mydriatics; while the remaining 5% is due to blockages of the drainage system due to inflammatory, hemorrhagic, trauma and tumor processes. It generally occurs over forty years of age and leads to loss of vision; it can constitute acute or subacute processes.
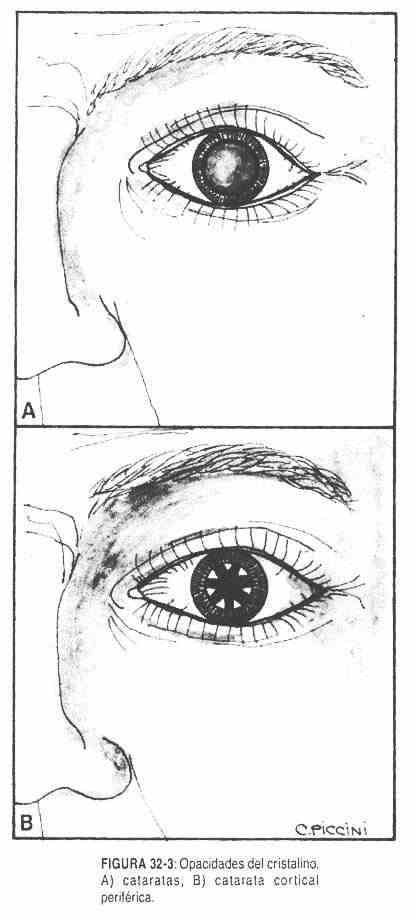
The lens can become cloudy, leading to cataracts (Figure 32-3, A), which can be congenital or acquired, unilateral or bilateral, central or cortical (Figure 32-3, B). They are common in diabetes mellitus, where high levels of sugar within the lens are transformed into sorbitol and alter the characteristics of the lens. Cataracts can also be seen in hypoparathyroidism, during treatment with corticosteroids, or chlorpromazine, in Wilson's disease, and in galactosemia. The lens, in addition, may be subluxed as occurs in the syndrome of
Marfan and in homocystinuria.
Sometimes there are hemorrhages in the vitreous humor that make vision difficult. They can also shed cells, giving rise to the appearance of so-called floaters.
Sensory disorders . When there is a decrease in visual acuity, with transparent means of refraction and that does not improve with corrective lenses, a sensory deficit should be suspected. The retina will be examined during the ophthalmoscopic exam.
Alterations in the ophthalmoscopic examination
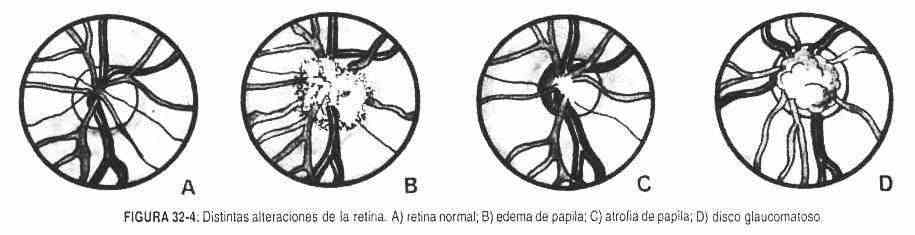 Disc alterations . Papilledema . The increased intracranial pressure is transmitted through the subarachnoid space to the periphery of the optic nerve. First, as the pressure increases, the venous pulsations disappear, which continues with engorgement and ends with loss or effacement of the edges of the papilla, which is observed protruding forward. These changes become more relevant in the temporal arc (Figure 32-4, B).
Disc alterations . Papilledema . The increased intracranial pressure is transmitted through the subarachnoid space to the periphery of the optic nerve. First, as the pressure increases, the venous pulsations disappear, which continues with engorgement and ends with loss or effacement of the edges of the papilla, which is observed protruding forward. These changes become more relevant in the temporal arc (Figure 32-4, B).
Papilla atrophy . It is produced by the death of the fibers of the optic nerve, with loss of the capillaries of the disc, which gives it a characteristic white color, with clear margins and an excavated disc. The arterioles are preserved at the level of the papilla (Figure 32-4, C).
Glaucomatous disc . In glaucoma, the disc is enlarged, which is pale, and an intradiscal area appears devoid of arterioles, which are seen displaced towards the nasal area (Figure 32-4, D).
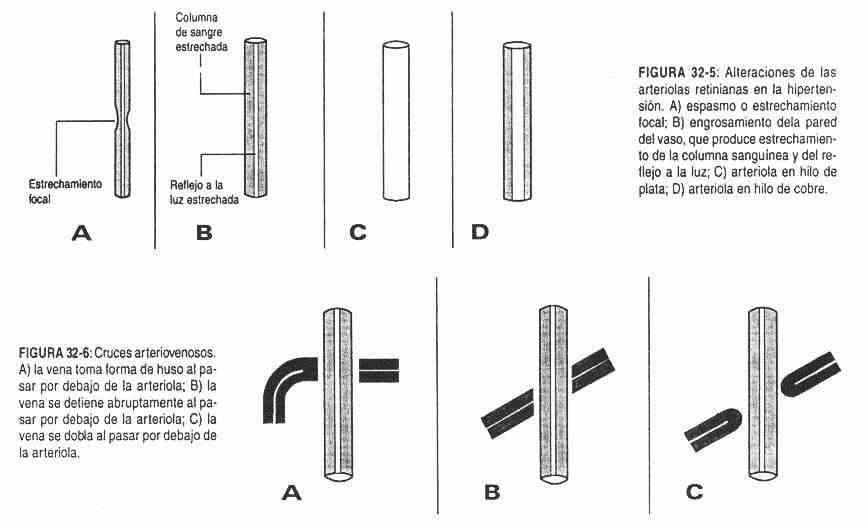
Alterations of the retina . Alterations of the arterioles . They can present narrowing, which produces a decrease in the reflection to light and a reduction in the caliber, showing the narrowed column of blood (Figure 32-5, A). If the narrowing is persistent, the wall of the vessel will thicken and will be less and less transparent. Reflection to light will be diminished (Figure 32-5, B). If the thickening is total, the blood column will no longer be seen, forming the arteriole in silver wire (Figure 32-5, C). In the central arterioles, near the disc, increased tortuosity and light reflection will form copper-wire arterioles. These changes occur in high blood pressure (Figure 32-5, D).
The arterioles may show thickening of the wall, with a decrease in the blood column and tortuosity. These modifications are seen in atherosclerosis.
Alterations of arteriovenous crossings . As the arteriolar wall thickens, it becomes firmer than normal, compressing the vein, causing first dilation and then disappearance of the vein below the arteriole (Figure 32-6). This is how it can be observed that the ends of the vein progressively disappear and move away from the artery path, losing sight of the intersection.
Retinal hemorrhages . The hemorrhages are frequently striated or linear, called flame, and are due to the presence of red blood cells accumulated in the sac that surrounds the nerve between two fibers. These changes occur in high blood pressure (Figure 32-7).
Deep haemorrhages appear as small, reddish, irregular, round or oval spots and are located in the deep plexiform layer. They are commonly seen in diabetes and consumption coagulopathies (Figure 32-7).
The rupture of arterioles in the most superficial or inner layer of the retina causes hemorrhages between the vitreous humor and the retina, called preretinal hemorrhages (Figure 32-7). They appear as small blood collections and are seen in diabetes and high blood pressure.
Microaneurysms are small reddish spots, about the size of a pinhead, usually seen near the macula. They are seen in diabetes. Roth spots have a white or pale center surrounded by a hemorrhagic halo (Figure 32-8). They are found near the disc and, despite having also been described in leukemia, kala-azar, and thrombotic thrombocytopenic purpura, they remain a very good sign of bacterial endocarditis.
Exudates . Plasma exudates are cottony and near the arterioles; they have a greyish whitish color. These are called soft exudates (Figure 32-9, A) and are seen in high blood pressure.
Hard exudates (Figure 32-9, B) are sharply edged, irregularly shaped, smaller, bright yellowish in color, and grouped. They are seen in diabetes and high blood pressure.
Colloid bodies are very small, round, yellowish, and related to aging (Figure 32-9, C).
Scarring chorioretinitis (Figure 32-9, D). It is a smaller lesion, with irregular borders delimited by pigments, and whitish or greyish in the central part.
It is the sequel to a healing process in the retina.
Degeneration of the receptor layer . It occurs in the outermost receptors and in the squamous epithelium. It occurs in Lawrence-Moon-Biedl syndrome, in progressive ophthalmoplegia, retinitis pigmentosa, Refsum's disease, in Kearns-Zayre syndrome, in juvenile lipid deposit disease or Batten-Mayou disease, and in senile idiopathic macular degeneration. It is seen as a form of chorioretinal atrophy and is diagnosed by retinofluorosceinography.
Bruch's membrane degeneration . In this case, there is proliferation of fibrous tissue, as in Paget's disease, acromegaly, elastic pseudoxanthoma, and hyperphosphatemia. It is observed as a zone of atrophy, thinner and paler
Phenothiazine degeneration . These drugs can be conjugated with melanin, causing degeneration of the outer layers of the retina. Atrophic areas are observed.
Hypertensive, diabetic and arteriosclerotic retinopathy . Elevated blood pressure levels can produce changes in the retina and retinal arterioles that are evident on ophthalmoscopic observation (Figure 32-10). The first change that occurs is the spasm of the vessels with a decrease in the caliber of the arterioles.
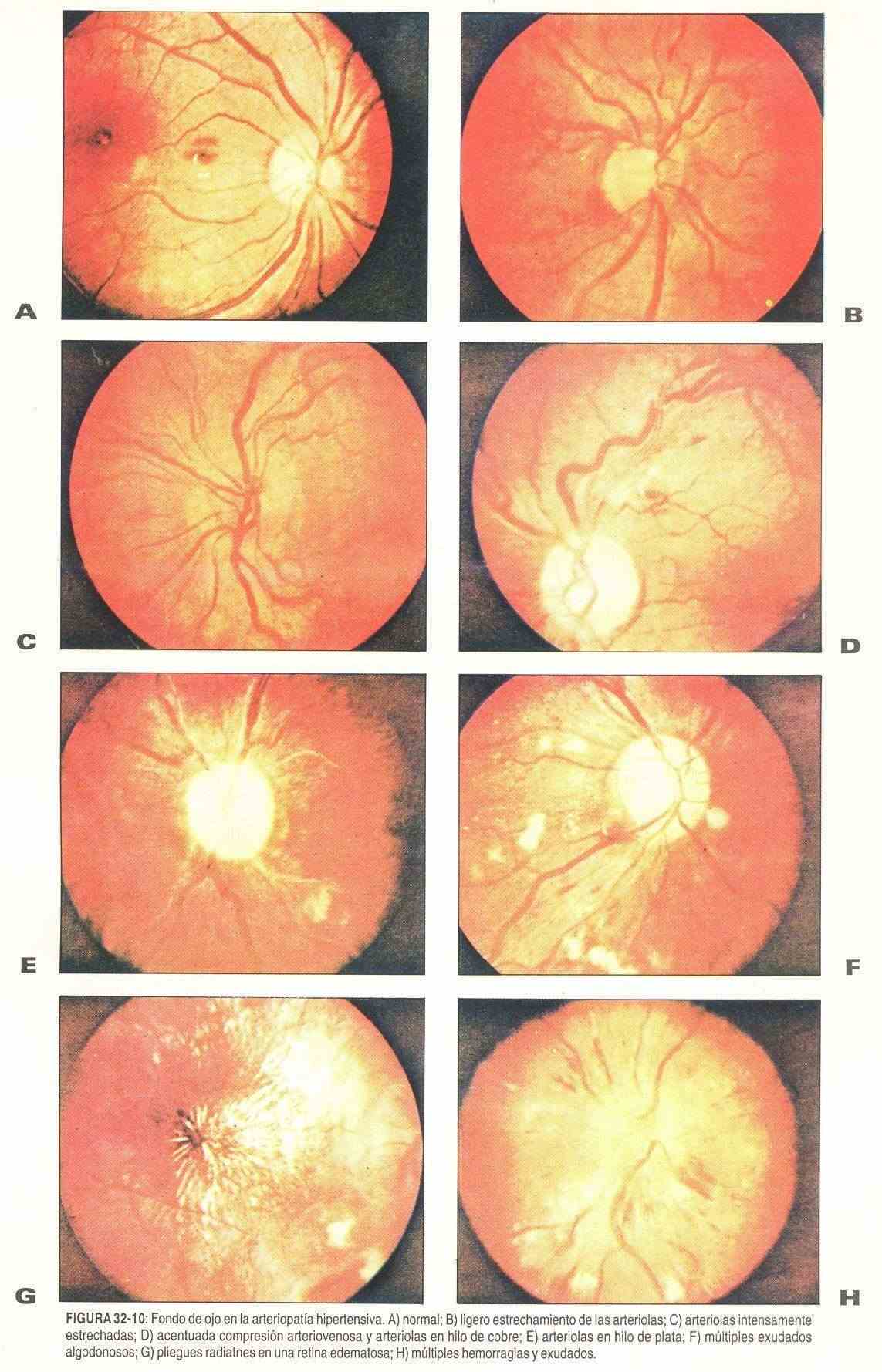
 In young patients with toxemia gravidarum and acute glomerulonephritis, the elasticity of the vessels allows the process to be self-limited, so that when the blood pressure level returns to normal, these changes disappear.
In young patients with toxemia gravidarum and acute glomerulonephritis, the elasticity of the vessels allows the process to be self-limited, so that when the blood pressure level returns to normal, these changes disappear.
When the pressure figures are maintained in a sustained way, as in benign hypertension, more important changes appear. These include: tortuosity of the vessels, arteriovenous compression or arteriovenous crossings, with production of the so-called copper wire and silver wire arteries.
In the patient with malignant hypertension, cottony exudates, hemorrhages, especially in flames, and papilledema appear.
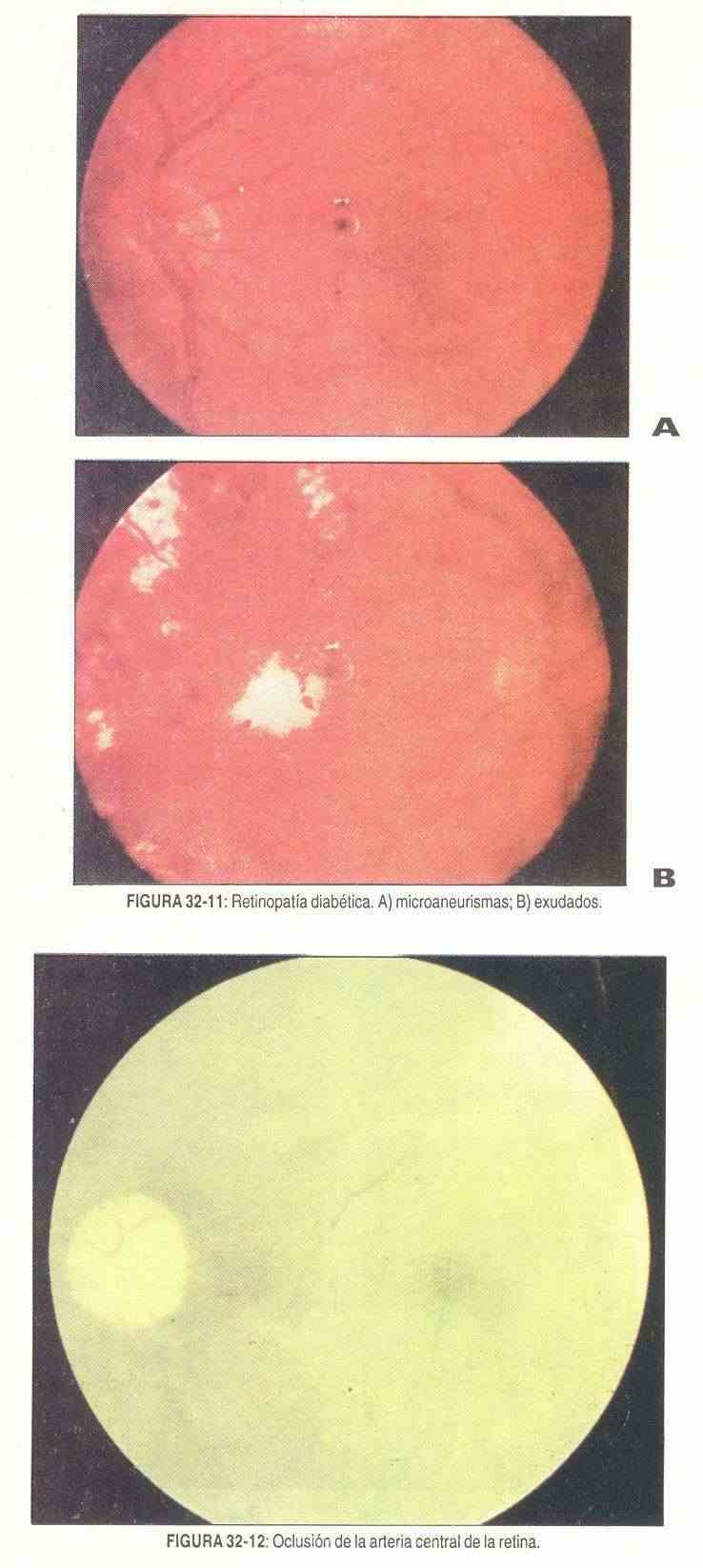
Diabetic retinopathy. Capillary microaneurysms are perhaps the most characteristic lesion associated with diabetes mellitus. Their presence seems to be more related to the duration of the disease than to the degree of control of it. They are presumably preceded by dilation of the retinal veins, which is difficult to identify. Today they are thought to represent saccular dilatations of the capillaries. The exudates in the diabetic appear on the periphery of the retina that forms an incomplete circle around the macula, called circinate retinitis that gives it a serous or cheesy appearance. Pinpoint hemorrhages and major hemorrhages can also be seen; are early-onset. The most advanced form of diabetic retinopathy is proliferative retinopathy, which is characterized by vascular proliferation or neoformation. It occurs in 10% of diabetics; it is a manifestation of a long evolution and is associated with greater visual loss (Figure 32-11).
Atherosclerotic retinopathy . In this disease, changes or alterations are observed at the level of the arterioles. Vascular tortuosity, together with the reduction of the arteriolar lumen and the formation of copper and silver wires, are the changes that are most frequently found; they are closely linked with high blood pressure. Arteriovenous crossovers become important when viewed a disk away from the disk.
Other alterations of the fundus . Retinal detachment may be found in recurrent polychondritis along with retinal edema, chorioretinal scars, and optic neuritis.
In systemic lupus erythematosus, it is possible to observe cottony exudates produced by microinfarcts in the nerve fiber layer of the retina. Manifestations of vasculitis can also be seen (sign of the sheath or of the pipe: two white, thin and parallel lines, with the arteriole of narrow caliber), papilledema, optic atrophy, etc. Rarely, similar lesions appear in systemic sclerosis, dermatomyositis, or polymyositis.
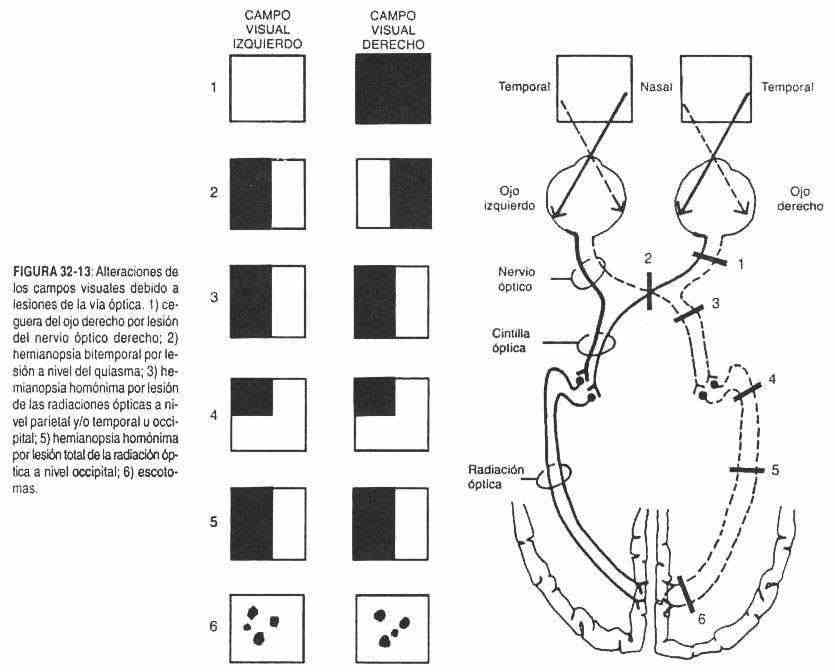
In 10-20% of patients with periarteritis nodosa there are changes in the fundus, similar to those that occur in systemic lupus erythematosus, to which occlusion of the central retinal artery may be added. These same changes can be found in Wegener's granulomatosis. 50% of patients with temporal or giant cell arteritis present ocular lesions; The most common cause of vision loss is ischemic optic neuropathy (Figure 32-12). The appearance of scotomas in the visual field is earlier.
5% of patients with histoplasmosis develop disc-shaped spots at the level of the macula, which begins with an accumulation of subretinal fluid or around old scars, with subretinal neovascularization, leading to scarring of the macular area.
53% of cases may have hemorrhages.
In acquired toxoplasmosis, chorioretinitis is seen; there is a great profusion of exudates, with the appearance of a cloud, and papilledema may appear. In the recurrent forms there are yellowish scars.
Lesions in the fundus of the eye are also seen in some anemias, such as sickle cell disease, where the alterations occur due to vascular thrombosis; retinal detachments may occur. In sarcoidosis, in addition to keratitis and episcleritis, it is possible to observe the deposit of sarcoidotic material in the retina. Other times, the presence of dark-colored retinal elevations or tumors should be taken into account, leading to the diagnosis of melanoma; if it is clear, it may be a metastasis, and if it is transparent, the most frequent cause is retinal detachment.
Visual field alterations
Various terms are defined below that will be helpful.
The visual field is the portion of space that can be seen by the eye, in a position of distant vision at the level of the eyeballs. The evaluation can reveal lesions in the retina, the optic nerve, the chiasm, the optic tracts, the external geniculate bodies, the optic radiation and the occipital cortex.
Amaurosis . It is blindness or total loss of vision. It can be permanent, as in optic nerve injury; or transitory, as in hysterical amaurosis; or fleeting, as occurs during platelet embolization from carotid atherosclerotic lesions.
Amblyopia . It is the decrease in visual acuity, not due to vision errors or another eye disease. It is observed in alcoholism and smoking due to damage to the optic nerve, due to a probable vitamin B12 deficiency.
Strachan syndrome (ambiopia, neuropathies, and orogenital dermatitis) occurs in undernourished populations.
Nictalopia . It is the loss of night vision, due to disorders of vitamin A or retinal pigmentation.
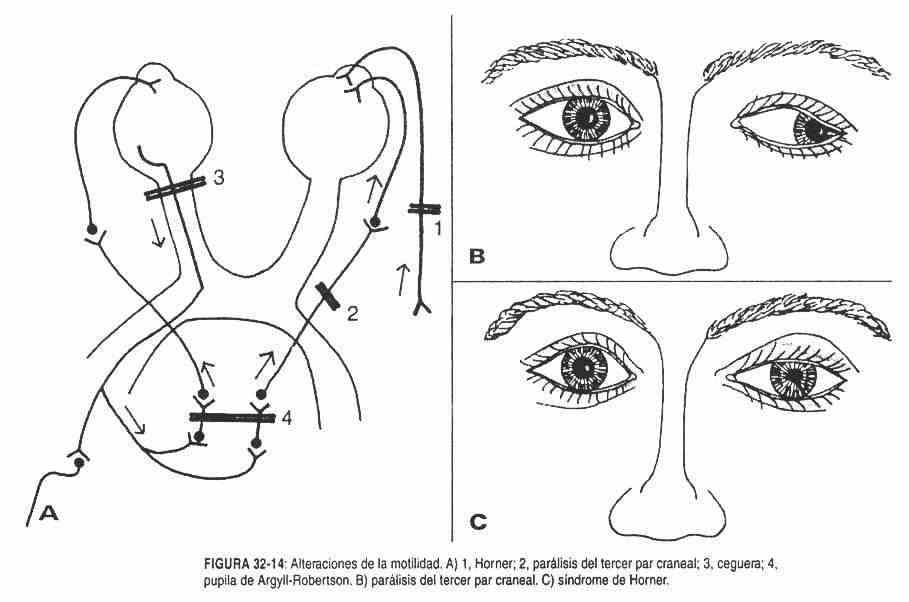
Hemianopia . It is the loss of vision in the middle of the visual field. They are called temporal or nasal according to the visual field lost and not according to the side of the injured retinas. They are called homonyms when visual fields on the same side are lost; a homonymous hemianopia does not see the nasal visual field on one side and the temporal field on the other. Hemianopsies are heteronymous when the amaurotic visual fields are the same; both nasal or both temporal.
Quadrantopsia . It is the loss of vision of a quarter of the visual field.
Scotomas . They are circumscribed areas of visual loss, and can be central or peripheral. There is a physiological scotoma at the level of the papilla. They are a frequent cause of papillitis and neuritis, and therefore of scotomas, demyelinating diseases such as multiple sclerosis, metabolic conditions such as diabetes, deficiency conditions such as beriberi (vitamin Bi deficiency), infections such as meningitis and polio, diseases caused by toxins such as tobacco, alcohol and lead, and ischemic neuropathies.
Metamorphopsia . It is the curved vision of straight lines; speaks in favor of a retinal injury, and is sometimes helpful in differentiating retinal injuries from occipital injuries. It is due to a scotoma in the macula, due to demyelinating, toxic or vascular diseases.
Tubular vision . It is the peripheral narrowing of the visual field, or shotgun-barrel vision, common in hysteria and in some organic diseases. In organic diseases, as the object moves away, the vision of it is greater; the opposite happens in hysteria.
Concentric constriction . It is due to an increase in the blind spot due to papillary edema.
According to the visual field defects, it is possible to obtain an orientation about the anatomical level of the lesion in the optic pathway. If the injury occurs at the level of the optic nerve (neuritis, tumors, ischemia) (Figure 32-13, 1), the corresponding visual field will be amaurotic. When the lesion is at the level of the chiasm (Figure 32-13, 2) (pituitary tumors, meningiomas, third ventricular and hypothalamic tumors) it produces a bitemporal hemianopia. If the lesion is located at the level of the optic tract (Figure 32-13.3) (tumors, a homonymous hemianopsia will occur; that is, the finding of a complete homonymous hemianopia means that the lesion is behind the chiasm. is incomplete (Figure 32-13, 4) (quadrantopsies), the lesion will be in the optic radiation at the temporal level and ' or parietal or occipital. If the quadrantopsia is homonymous, the lesion is likely occipital. If the optic radiation injury occurs at the parietal level, where the nerves come from the upper part of the retina, the quadrantopsia will be lower, and if they are affected in their temporal path, where the fibers come from the lower retina, quadrantopsia will be higher.
The total lesion of the optic radiation (Figure 32-13.5) produces a homonymous hemianopia, a defect similar to that caused by the lesion of the optic tract. When the lesion of the girdle or radiation is total or complete, macular vision is lost. In contrast, when the injury is incomplete, macular vision is often preserved. Horizontal hemianopsies are common in lesions of the occipital lobe, above or below the calcarine fissure.
Visual agnosia is an alteration of visual perception, in which the patient, although he sees objects, is unable to recognize them by name. The inability to recognize written words or letters is called alexia.
These alterations occur when there are lesions of the cortex in the secondary and tertiary visual cortical areas, located in front of the primary area of vision and in the angular gyrus of the dominant hemisphere. Micropsia and macropsia are the reduced or enlarged vision of objects. When it is unilateral, retinal disease will be considered, and if it is bilateral, the lesions will be temporary.
Color vision disturbance or dyschromatopsia
They can be of congenital or acquired origin. The most frequent cause of congenital dyschromatopsies is color blindness of congenital dyschromatopsies is recessive inherited color blindness, linked to the X chromosome, and therefore suffered only by men. In the different types of color blindness there are different blind colors according to the wavelengths affected.
Cranial nerves III, IV and VI (common ocular motor, pathetic and external ocular motor)
Among the anomalies of these cranial nerves, the alterations of motility and conjugated movements should be described.
Motility disorders
Eyelid ptosis . It is the total or partial drop, uni or bilateral, of the upper eyelid. It can be produced by:
Third nerve palsy partially controlling the elevation of the upper eyelid.
It can be of viral, metabolic origin (diabetes, toxic), syphilitic or secondary to a traumatic lesion of the sphenoid cleft, meningioma of the minor wing of the sphenoid, carotid aneurysm at the level of the cavernous sinus and due to injury to the nuclei of the III nerve , for vascular or tumor causes.
Paralysis of muscular origin . The cause is a familial ocular myopathy or myasthenia gravis.
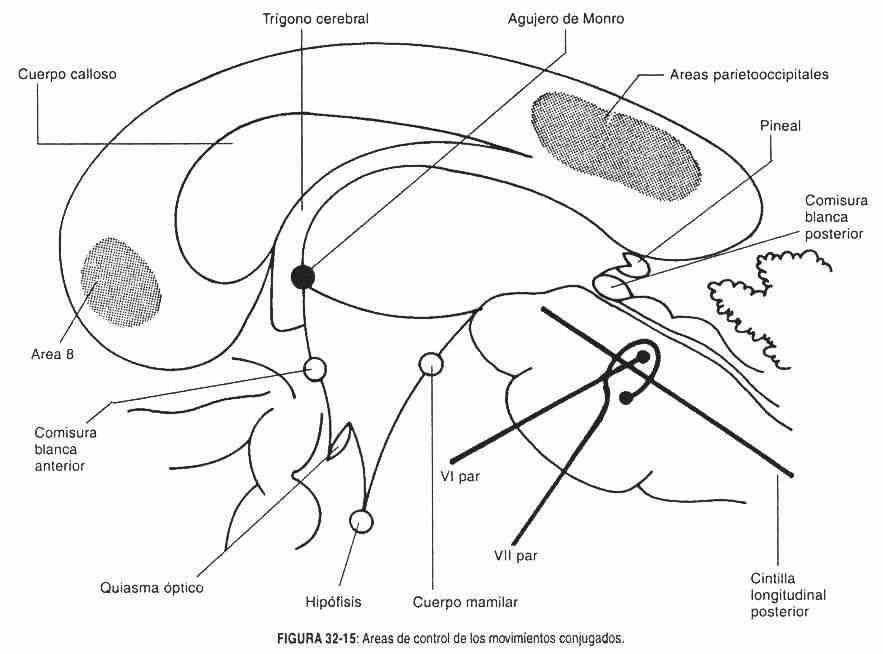
Sympathetic nerve injury . The smooth muscle tone of the eyelids is lost. It is produced by injury to the inferior sympathetic ganglion or stellate ganglion by a tumor of the pulmonary apex, causing the Claude Bernard-Horner syndrome (Figure 32-14, C) (ptosis, miosis, and enophthalmia) and loss of sensation on the affected side. When there is irritation at the level of the stellate ganglion by a tumor of the pulmonary vertex, lagophthalmia, mydriasis and exophthalmia occur, constituting the Pourfour du Petit syndrome.
 Paralysis of the III par . Third nerve palsy causes mydriasis, ptosis, and outward deviation of the eyeball (Figure 32-14, B). Cranial nerve palsies, depending on the level of injury, can be nuclear, supranuclear, and infranuclear. In common ocular motor palsies, infranuclear lesions are accompanied by complete paralysis, while nuclear and supranuclear lesions may not be complete and involve an isolated group of muscles. Weber syndrome, due to lesion of the corticospinal pathway of the midbrain of vascular or tumor origin, is characterized by alternating or crossed hemiplegia and ophthalmoplegia.
Paralysis of the III par . Third nerve palsy causes mydriasis, ptosis, and outward deviation of the eyeball (Figure 32-14, B). Cranial nerve palsies, depending on the level of injury, can be nuclear, supranuclear, and infranuclear. In common ocular motor palsies, infranuclear lesions are accompanied by complete paralysis, while nuclear and supranuclear lesions may not be complete and involve an isolated group of muscles. Weber syndrome, due to lesion of the corticospinal pathway of the midbrain of vascular or tumor origin, is characterized by alternating or crossed hemiplegia and ophthalmoplegia.
In Benedikt syndrome, the corticospinal tract or pathway, the red nucleus and the junction of the quadrigeminal tubercles with the thalamus (conjunctival tract) are injured, with signs of alternate or crossed cerebellar ataxia, with ophthalmoplegia and pyramidal signs.
In Claude Bernard-Horner syndrome there are lesions of the conjunctival arm and the red nucleus; the patient presents with ophthalmoplegia and crossed cerebellar ataxia.
In Nothnagel syndrome, the cerebellar peduncles and tectum are injured, with cerebellar ataxia and ophthalmoplegia.
Paralysis of the IV pair . It is manifested by the inability of the eyeball to look down and inwards. This pair does not carry parasympathetic fibers. It is a paralysis that is not frequent, and in which the patient compensates the presence of diplopia with a rotational movement of the neck. In nuclear lesions of this nerve, the paresis or paralysis of the greater oblique occurs on the opposite side to the lesion, in contrast to infranuclear lesions which occur on the same side as the lesion. Myasthenia gravis and other causes of exophthalmos should be ruled out.
VI nerve palsy . VI nerve palsy is manifested by deviation of the eyeball inward, with the inability to bring it out. It can be an early sign of intracranial hypertension, because the fibers of the sixth nerve travel an extensive path at the base of the skull.
The sixth nerve palsies or paresis, when the lesion is peripheral or infranuclear, are ipsilateral and complete; and when they are nuclear they are accompanied, by causes of close proximity, by lesions of the VII pair.
Infranuclear or peripheral palsies of these three cranial nerves can be due to aneurysms of the polygon of Willis, the cavernous sinus (FOix syndrome), skull base fractures, meningiomas, viral diseases (herpes), etc.
Ophthalmoplegia can be part of the migraine syndrome, with involvement of both the common ocular motor and the sixth nerve.
The palsies of pairs III and VI should suggest, when they occur in a child, in pons, and when they occur in an adult, in metastatic tumors of the rhinopharynx. One-sided paralysis that affects multiple pairs, with the characteristic of being painful, constitutes the Tolosa-Hunt syndrome, caused by a parasellar granuloma. The pain is produced by compromise of the 5th pair.
Conjugated movements alterations . Conjugated movements are the movements of the eyes that are carried out simultaneously and in the same direction. They are controlled by area 8 of the frontal lobe, the parieto-occipital areas, the posterior longitudinal band or median longitudinal fasciculus, and the pontine paraabducens region that is in the vicinity of the nucleus of the sixth nerve or abducens nucleus (Figure 32-15).
The posterior longitudinal band has intersegmental association fibers, between the bulboprotuberancial motor nuclei, the quadrigeminal tubercles and the sensitive cordonal cells. It descends through the internal capsule; it is always in front of the ependymal cavities, and when descending to the pons it decuses in front of the nucleus of the sixth pair. It is responsible for the coordination of eye movements, so that the vision is unique.
The front area 8 controls fast, ballistic movements that change the gaze with a speed of 700 ° per second. A seizure involving that area directs the eyes to the opposite side. On the other hand, in the destructive lesion of area 8 the deviation of the eyes towards the same side will deprive. This alteration is early. When the stimulus covers the two frontal areas, the eyes move up and down. If there is injury in both frontal areas, the eyes will not be able to move voluntarily.
The parietal and occipital regions control slow and tracking movements. His injury causes the loss of these movements and optokinetic nystagmus towards the injured side.
Different pathological processes can act on the areas and pathways that control conjugated movements from the cortex to the ocular motor nuclei and the paraabducens region and on the pathways that control said movements. They can be vascular, tumor or degenerative lesions (eg: multiple sclerosis).
 Damage to both frontal areas or their descending pathways makes voluntary active motility of the eyes impossible with preservation of visual reflexes. It is the picture in which, when bending the head, the eyes turn to the opposite side. This condition is called ocular apraxia.
Damage to both frontal areas or their descending pathways makes voluntary active motility of the eyes impossible with preservation of visual reflexes. It is the picture in which, when bending the head, the eyes turn to the opposite side. This condition is called ocular apraxia.
Lesions of the posterior longitudinal band (due to compromise of the pathways of the photomotor nucleus of the III pair or nucleus by Edinge and Westphal), at a high level, near the posterior commissure, will produce fixed pupils with impossibility of conjugated gaze upwards and towards down, may or may not be accompanied by alterations in convergence movements. If there is damage to the internal rectus nucleus pathways, and also to the common ocular motor, Parinaud's syndrome occurs, frequently caused by pinealomas.
Injury to the paraabducens region results in ipsilateral gaze paralysis, and consequently the eyes look to the opposite side of the injury. The paralysis of the conjugated movements and of some motor nucleus always indicate that the lesion is at the pontine or pedicle level.
When the lesion is at the pedicle level, at a lower height than that of Parinaud's syndrome, loss of convergence occurs, with paralysis of the internal rectus. In this case, there is alteration of both the conjugated movements and the mobility of the internal rectum due to partial nuclear damage of the third nerve.
If the lesion is pontine, the nuclei of CN III are not affected, but CN VI and lateral conjugate movements may be compromised. In this case, the patient is unable to abduct with the eye on the injured side and to adduct with the opposite.
Pictures are described where only the posterior longitudinal band is affected, in which the adduction of the opposing eye is absent and there is nystagmus on the injured side when the patient abducts (internuclear ophthalmoplegia). This injury can be unilateral or bilateral. When the lesion is unilateral, it is located on the side in which the adduction is most noticeable.
Other disturbances of eye movements .
Clonus . It is an irregular, sustained and conjugated movement of the eyes in a lateral or vertical direction, as if it were a dance. It is seen in cerebellar diseases, viral diseases, and hemorrhagic fever.
Flutter . It is a horizontal, brief and intermittent movement of the primary position of the gaze. It is also seen in viral processes. It has a lower hierarchy as a symptom.
Dismetria . It is a movement that occurs with the fixation of the gaze, of overshot of the eyeball. It is produced by cerebellar disease; after overshoot, rapid oscillations of decreasing amplitude are observed until fixation is reached.
Pupil alterations
The pupil can have alterations in its size, shape, symmetry and reflections.
Miosis . It is the constriction of the pupil (Figure 32-16, A), with a diameter less than 2 mm. It is produced by irritative action of the parasympathetic, or by injury to the sympathetic, or by action of drugs at the level of the autonomic nervous system. It can be uni or bilateral.
Causes of miosis . The destruction of the sympathetic system or the stimulation of the parasympathetic system at any of its levels, by toxic, tumor or degenerative processes (multiple sclerosis), produces miosis. When the sympathetic system is completely affected, due to lesion of the stellate ganglion, miosis, lack of sweat on the forehead and neck and red eye occurs, constituting the Claude Bernard-Horner syndrome.
Likewise, some chronic diseases (syphilis) and bilateral, drugs (barbiturates, morphine, etc.) cause unilateral miosis. Extreme constriction, with bilateral miosis, will be seen in pontine lesions, possibly due to compromise of the pupillo-dilating fibers.
Mydriasis . It is the dilation of the pupil with a diameter greater than 4 mm (Figure 32-16 E
It is produced by irritation or stimulation of the sympathetic nervous system, or by injury to the parasympathetic nervous system. It can be uni or bilateral. When it is unilateral, it is called anisocoria.
Causes of mydriasis . The destruction of the parasympathetic system or the irritation of the sympathetic system, in any of its cerebral or peripheral levels, or by the action of drugs (alcohol, marijuana), will produce mydriasis. Unilateral mydriasis, with lagophthalmia and exophthalmos, and sweating of the face and neck on the affected side, is known as Pourfour du Petit syndrome. Bilateral mydriasis with loss of reflexes is frequently seen in midbrain lesions and is a common finding in deep comas. Cocaine dilates the pupils by inhibiting the reuptake of norepinephrine in nerve endings, as does glutetinide, which also causes mydriasis.
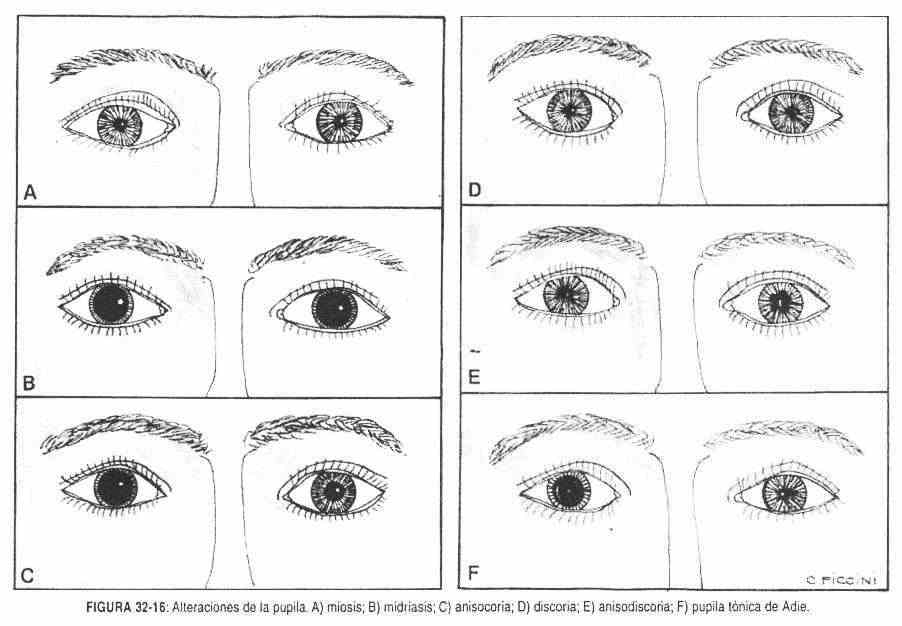
Anisocoria . It is the dilation of a pupil, with loss of equality between the two (Figure 32-16, C). Essential anisocoria is a congenital anisocoria, with normal pupillary responses.
Discoria . It is the loss of regularity in the normal circular shape of the pupil. Its most common cause is lens surgery (Figure 32-16, D).
Anisodiscoria . It is the presence of a larger pupil, with alterations in its shape (Figure 32-16, E).
Reflex disorders
When a blind eye is stimulated due to a lesion of the retina or the optic nerve, no pupillary response is obtained in that eye, nor a consensual response in the other eye, due to loss of the optic pathway in the reflex arc of the photomotor and consensual reflexes. When the healthy eye is stimulated, a pupillary response is obtained with this eye, and consensual in the diseased eye, due to the integrity of the common ocular motor nerve.
Loss of the photomotor reflex and persistence of the accommodation reflex is called the Argill-Robertson pupil (Figure 32-14, A). Sometimes it coexists with atrophy of the iris and with small and uneven pupils. It is seen in syphilitic meningitis and other forms of late syphilis, such as tabes dorsalis. The likely site of injury is in the vicinity of the nucleus of CN III, where the pupillo-dilating parasympathetic fibers are found close to the reflex arc fibers.
The Argyll-Robertson pupil can also be seen in other processes that injure the midbrain: pinealoma, multiple sclerosis, and diabetes mellitus.
Other times there is a tonic constriction of the pupil with inability to accommodate, and blurred vision may occur. The pupil does not contract or contracts little with light stimulation, although it can do so slowly with maximum light stimuli and with diluted pilocarpine, which usually will not affect a normal person. This pupil can be seen dilated or contracted and is in this state for a few minutes. It is the so-called pupil of Adié (Figure 32-16, F). It is produced by injury to the postganglionic parasympathetic fibers. It is more common in women, and unilateral in 80% of cases.
In hyperthyroid syndrome, pupillary reflexes can be altered, as well as oculomotor movements. In retroocular expansive processes it is possible to observe similar alterations. Eyelid palsies can obstruct vision, as occurs in Kiloh and Nevin ocular dystrophy and oculopharyngeal dystrophy.
Strabismus . It is a defect in the action of the muscles of the eye, which can be convergent when the crossed eye is deviated out), or alternating, unilateral or bilateral, transitory or permanent. Strabismus is closely related to refractive phenomena, and its symptom may be diplopia. The adult with strabismus has diplopia because his visual defect has developed in adulthood, whereas in strabismus at birth there is no double vision because diplopia has been inhibited in the deviated eye. The farsighted person presents convergent strabismus, and the myopic divergent.
Strabismus is often seen in infants when they begin to stare. And in abnormal conditions it can be produced by a disorder of the means of refraction, or by a disorder of the muscles, either by disease or by injury to the nerve pathway.
Strabismus can be paralytic or nonparalytic. Paralytic strabismus is manifested by the inability to move in the direction in which the muscle or nerves are affected. It becomes apparent only when trying to move the eyeball to the affected side. In nonparalytic strabismus, the eye is permanently deviated and is usually caused by ophthalmological problems.
To evaluate small ocular deviations, the occlusion or occlusion coverage test is performed. With the ball of the big toe, the examiner alternately covers the patient's eyes, asking him to look at a fixed point. It begins by covering one eye and the uncovered eye is observed; If the open eye does not move, there is no squint in that eye. In this same case, if there is a strabismus, when uncovering the covered eye, a movement will be observed to regain its original position, which indicates the action of the fusion reflex to preserve binocular vision.
The Hirschberg test is performed with a light in the middle of the observer's eyes, asking the patient to observe this light. The light reflection will appear symmetrically at the level of the patient's corneas. The patient is then asked to turn his head to the left and to the right, always observing the light beam. If the light beam leaves the cornea, outwards or inwards, it is in the presence of a convergent or divergent strabismus.
Pair V or trigeminal nerve
The patient may present alterations in sensation, motor skills and reflexes.
Sensitivity alterations . There may be decreased sensitivity (anesthesia, hyperesthesia) or pain in the territory innervated by the sensory branches (trigeminal neuralgia, postherpetic neuralgia, Costen syndrome, Tolosa-Hunt syndrome, Raeder's paratrigeminal syndrome).
Anesthesia and hypoesthesia can occur in pons lesions, either at the level of the nuclei or the descending pathways. In cerebellopontine angle tumors, there is hypoesthesia or anesthesia.
In hysteria, due to conversion mechanisms, hypoesthesia or anesthesia of the region can be observed. In these cases there is no atrophy and the reflexes are preserved.
Anesthesia in this area can be induced by the use of stilandeine, long used to treat Kala-azar and multiple melanoma, and by inhalation of trichloroacetic acid vapors. In the recovery phase, pain may occur. When there is bilateral trigeminal anesthesia, leprosy should be suspected. A benign trigeminal neuritis, chronic or acute, has also been described, associated with lupus erythematosus, progressive systemic sclerosis, Sjögren's syndrome, and in some cases Horner's syndrome.
Gradenigo syndrome, due to anterior petrous lesions, shows painful lesions at the level of the Gasser ganglion and alterations of the sixth nerve.
Pain in the temporomandibular joint is called Costen syndrome. Raeder's paratrigeminal syndrome includes frontotemporal and mandibular pain. In postherpetic neuralgia, the antecedent or appearance of stellar vesicles in the path of the affected nerve is important.
Motor disorders . The absence of contractions of the masseter or the temporal bone or the lack of laterality movements reveal defects in the motor skills of the 5th pair, as well as the lack of blinking.
Lockjaw consists of the tonic spasm of the chewing muscles, and is symptomatic of tetanus. It can also be seen by the use of phenothiazines and in diseases of the teeth, jaws and neighboring tissues.
Reflex alterations . They can be found in trigeminal nerve lesions, corneal, conjunctival, masseteric and corneomaxillary reflex alterations.
The corneal and conjunctival reflexes can be abolished by lesions at the level of the cavernous sinus (aneurysms, thrombosis, granulomas). It is accompanied by ophthalmoplegia and sensitivity alterations in the ophthalmic territory. It is produced by injury to the oculomotor nerves and the ophthalmic branch of the trigeminal nerve. When there is pain, it constitutes Tolosa-Hunt syndrome.
The masseteric reflex may be accentuated in pseudobulbar syndrome due to injury to the corticonuclear pathway. Nuclear lesions produce the abolition of this reflex.
The corneomaxillary reflex is a pathological reflex, which occurs when the cornea is stimulated and which causes a deviation of the lower jaw towards the unstimulated side. It manifests as a lesion of the corticonuclear pathway.
In the sphenoid cleft syndrome, cranial nerves III, IV, V and VI are affected, coexisting motor and sensory alterations with alterations in the pupillary reflex. It is produced by tumors of the sphenoid or aneurysms at that level.
Pair VII or facial nerve
There may be alterations in taste, in the motor skills of the mimic muscles, and in the trigeminofacial reflexes.
Alterations of taste . The taste sensations of the anterior two thirds of the tongue are conveyed by the facial nerve. Ageusia is called the absolute lack or loss of the sense of taste; hypogeusia is the diminution of taste and parageusia the perversion of taste.
A common cause of loss of taste after trauma is a skull base fracture. The patient consults for loss of taste, although it is usually associated with a loss of the sense of smell.
Complete loss of taste sometimes results from bilateral nerve VII lesions; although the most frequent is the lesion of the taste corpuscles that occurs in atrophic glossitis, in mycoses and in desquamative lesions of the tongue that are accompanied by dryness.
In CN VII paralysis, ipsilateral ageusia of the middle of the tongue is found.
Decreased taste sensations may be associated with contralateral parietal and thalamic lesions. Stimulation of the anterior area of the secondary sensorimotor cortex produces an increase in taste. A gustatory aura can be the beginning of a seizure originating from that territory. It can also be part of an uncinate seizure, and if it coexists with auditory or visual hallucinations and a dream state, the seizure stimulus will have extended laterally and rostrally from the uncus. They can coexist with olfactory hallucinations in some organic conditions (encephalitis) and in psychoses. Parageusia can occur due to the action of certain medications during the treatment of psychoses. Haloperidol exacerbates hallucinations.
Motor disorders . Motor alterations can be caused by lesions of the cortical and nuclear pathways, constituting central paralyzes, or by nerve damage, leading to peripheral paralyzes.
The peripheral lesion characteristically takes both the upper facial nerve and the lower facial nerve. In this case, the plegic half-face does not present wrinkles on the forehead, the lip corner is drooping, the lower eyelid is sunken, and the palpebral fissure cannot be closed; by asking the patient to close his eyes, the paretic side will not close, and the eyeball will deviate upward (Bell's sign); or when asked to look up, the paired eyeball will rotate more clearly (Nigro's sign). Food collects between the lips and teeth, and saliva runs off the corner of the mouth (Figure 32-17, A).
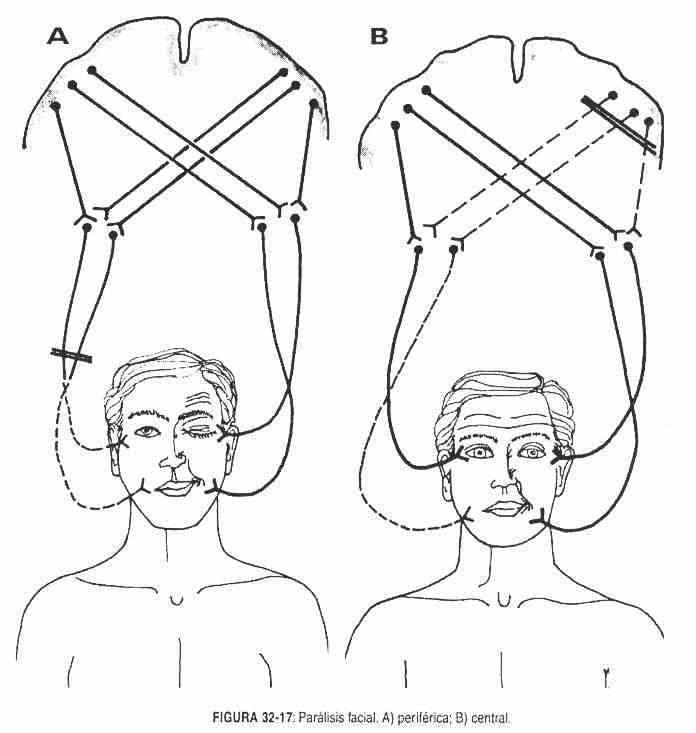 If the lesion is above the entrance to the chorda tympani nerve, loss of taste is added to the previously described signs. If this lesion is at the level of the geniculate ganglion, the decrease in tears will be added, and there may or may not be alterations corresponding to the VIII pair (tinnitus, deafness or dizziness). They frequently occur due to inflammatory affection (of undetermined origin) of the nerve or in its vicinity, around the stylomastoid foramen.
If the lesion is above the entrance to the chorda tympani nerve, loss of taste is added to the previously described signs. If this lesion is at the level of the geniculate ganglion, the decrease in tears will be added, and there may or may not be alterations corresponding to the VIII pair (tinnitus, deafness or dizziness). They frequently occur due to inflammatory affection (of undetermined origin) of the nerve or in its vicinity, around the stylomastoid foramen.
Sometimes aberrant nerve regeneration occurs, resulting in abnormal innervation. Thus, when you want to contract the orbicularis oculi, for example, the corner of the mouth contracts, or when a facial muscle contracts, tears are produced (crocodile tears), or when you eat there is tear activity (Bogorad syndrome) .
Recurrent or permanent facial paralysis is rarely combined with particularly labial edema, and tongue plication is occasionally seen. It is the so-called Melkersson syndrome, of unknown etiology, and sometimes linked to leprosy. In herpes zoster of the geniculate ganglion (Ramsay-Hunt syndrome), severe facial paralysis, vesicles in the pharynx and in the external auditory canal, and sometimes involvement of the eighth nerve are observed.
Sometimes it occurs bilaterally and successively. 75% of peripheral facial paralyzes recover.
The central lesion (Figure 32-17, B) will produce disorders in the territory innervated by the lower facial, not observing alterations in the upper facial territory, due to the contralateral and ipsilateral supranuclear cortical connections that only the upper facial nucleus has. whereas the nucleus of the upper facial, while the nucleus of the lower facial has only contralateral supranuclear connections. The most common causes are hemorrhages and tumors.
When you close your eyes, they close but weakly. When looking up, wrinkles occur all over the forehead.
Combined syndromes where the VII par . Some tumor or infectious processes of the internal auditory canal will produce symptoms corresponding to the VII and VIII cranial nerves.
The acoustic neurinomas or meningiomas that develop at the level of the cerebellopontine angle, alter the pairs, V, VII and VIII and sometimes the IX pair.
A mass in the lower part of the pons, at the level of the nucleus of the VII nerve and sometimes accompanied by lesions of the sixth nerve, produces facial paralysis, paralysis of the external rectum, and contralateral hemiplegia. Sometimes it is accompanied by paralysis of the gaze towards the injured side (Millard-Gubler syndrome).
Trigeminofacial reflex alterations . Both the nasopalpebral and supraorbital reflexes, as well as the blink reflex, can be altered in peripheral lesions of the facial nerve.
Chvostek sign . It is a pathological reflex, which is produced by stimulating the preauricular or masseteric region, and is manifested by the contraction of one or more facial muscles. It is present in hypocalcemia of any etiology
Pair VIII or auditory nerve
Alterations can occur in the auditory branch and / or in the vestibular branch.
Auditory branch disorders
Hearing loss is called hearing loss; Anacusis, also called deafness, is the loss of hearing, while presbycusis is the decrease in hearing for high tones, which occurs in the elderly.
Hearing loss. Sorderas . There are two types of hearing loss: conductive and perceptual or sensorineural.
Conduction hearing loss . In this case, there are difficulties for the sound to be conducted to the cochlea; problems are found in the outer and middle ear, such as: a cholesteatoma, occlusion of the external auditory canal, otitis media, or otosclerosis.
In these hearing loss, the Weber test is lateralized towards the diseased ear, because bone conduction is better than air conduction, which is why in the Rinne test the tuning fork is not heard when it is moved from the mastoid process to the canal. external auditory (Figures 20-3 and 20-4). Audiometry will demonstrate hearing loss for low tones (between 128 and 1024 cycles / sec). Signs for the airways and bone are reproduced in the Fowler's schematic or figurine (Figure 32-18).
The eyes represent air conduction, a circle for the right eye and a cross for the left; bone conduction is represented by the ears, with the angle directed towards the corresponding side. The left audiometric curves are drawn with these symbols in blue, and the right ones in red.
Perceptual or sensorineural hearing loss. In these hearing loss there is difficulty at the level of the inner ear (cochlea, cochlear division of the VIII pair or in its central connections) for the sound to be conducted to the auditory centers.
The Weber test is lateralized towards the healthy side and, as the lesion is in the nerve path, air conduction exceeds bone conduction, which is why in the Rinne test the tuning fork is generally heard better in the ear than in the mastoid.
The most frequent causes are presbycusis and lesions of the auditory nerve, tumorous (neurinoma), toxic (aminoglycosides and salicylates), traumatic (repeated acoustic trauma) and vascular (vertebrobasilar insufficiency).
A series of genetic transmission syndromes with sensorineural hearing loss (Hollgren, Refsum, Treacher-Collins and Waardenburg diseases) associated with mental disorders, changes in skin pigmentation, other skin abnormalities, etc. are also described. .
Hysterical deafness . It is difficult to recognize. The distinction can be made through the cochleoorbicular reflex, by which a blink occurs before an intense sound, or also through an intense sound that will cause sweating of the skin. They can be distinguished with an audiometer, with both ears connected, or with a stethoscope placed on both ears of the patient, whispering into the bell, and closing one pathway by occluding the rubber and then the other, without the patient knowing it.
There are other more sophisticated procedures to differentiate hysterical and simulation deafness.
Tinnitus or tinnitus s. It consists of a purely subjective phenomenon, characterized by a buzzing, chime or cricket songs. It is any sensation of sound for which there is no source of production outside the individual. It can accompany Méniére's disease, or the use of salicylates or quinine.
Vestibular branch disorders
The study of the vestibular branch includes nystagmus (see Chapter 19), the evaluation of the static coordination capacity and the dynamic coordination during movement.
Static coordination . Romberg's sign . In the patient with labyrinthine lesions or profound sensitivity alterations, suppressing vision control causes a fall to the ground.
This test is called a positive (+) Romberg test. In labyrinth syndrome there is a delay in the appearance of oscillations. Romberg's sign can be seen in tabes dorsalis, pernicious anemia, sirignomyelia, labyrinthine lesions of infectious cause (acute labyrinthitis), Méniére's disease, labyrinthine toxicity caused by drugs (aminoglycosides), multiple sclerosis, ataxia Friedreich's and other forms of spinocerebellar degeneration.
Dynamic coordination . Babinski Star March . The patient is asked to walk with his eyes closed four to five steps backward and four to five steps forward, and so on. A deviation of the march is observed until drawing a star on the ground.
This type of gait is typical of patients with labyrinthine syndromes.
Rademaker test . The patient is placed on a stretcher in the genupectoral position, supported by the palms of the hands. When mobilizing the stretcher, the patient will not adapt his body to maintain balance, and will fall easily.
Pair IX or glossopharyngeal nerve
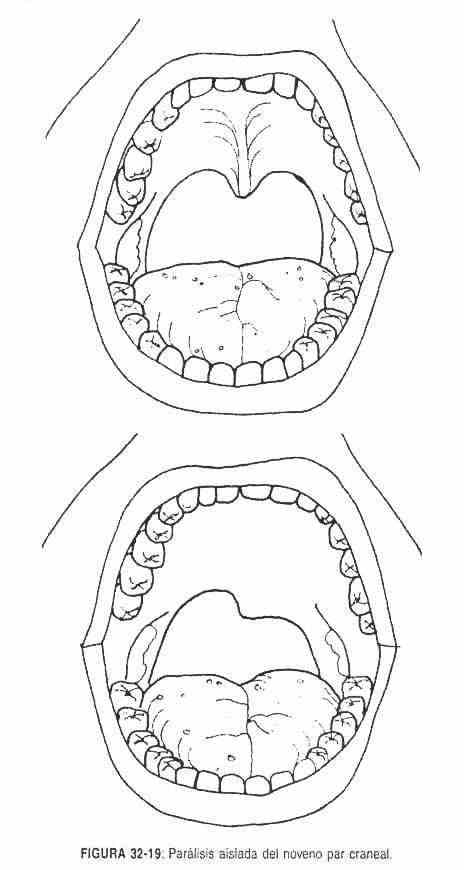 When listening to the patient's voice, the presence of a nasal voice (palsy of the IX pair) or of hoarseness, due to paralysis of the X pair should be evaluated. The IX pair can present alterations of the motor skills, the sensitivity and in the taste.
When listening to the patient's voice, the presence of a nasal voice (palsy of the IX pair) or of hoarseness, due to paralysis of the X pair should be evaluated. The IX pair can present alterations of the motor skills, the sensitivity and in the taste.
Motor disorders . In cases of isolated palsy of the ninth nerve, a descent of the soft palate with deviation of the raphe and the uvula towards the healthy side is observed when the patient says "a" (Figure 32-19). Swallowing may be impaired. The gag or pharyngeal reflex will be abolished in peripheral nerve lesions. In diphtheria there is paralysis of this cranial nerve, as in sarcoidosis, and in general combined with alterations of other cranial nerves.
Sensitivity alterations . Glossopharyngeal neuralgia is characterized by severe, paroxysmal pain in the pharynx and tonsils or in the ear, which is why it is more appropriately called vagoglossopharyngeal neuralgia. It is the only craniofacial pain that is accompanied by bradycardia and sometimes syncope. Spastic pains start when swallowing, but also when talking, chewing or laughing. This picture should be distinguished from that caused by tumors (carcinomas, epitheliomas) of the oroinfracranial or peritonsillar region, which produce pain indistinguishable from neuralgic pain. The glossopharyngeal can rarely be affected by shingles.
Alterations of taste . The posterior third of the tongue is innervated by CN IX (see taste disturbances described with CN VII).
Salivation disorders . The aforementioned alterations can coexist with disorders in salivation.
X pair or pneumogastric nerve
Pneumogastric injury can occur alone or in association with injuries to other cranial nerves or nerve pathways. These accompanying injuries will serve to locate the level of injury.
The paralysis of the X pair will produce a hoarse voice, with ipsilateral sagging of the soft palate, and loss of the gag reflex. The voice has nasal characteristics, and there may be loss of sensation in the external auditory canal and pinna. Central lesions are accompanied by cerebellar signs and loss of sensitivity to pain and temperature. If the injury is extramedullary, there will be deficient signs in other cranial nerves, depending on the site of the damage (posterior torn foramen, retroparotid space). Alterations of the great vessels (aneurysms) and tumor processes of the left pulmonary hilum are a frequent cause of ipsilateral recurrent nerve palsy, producing a two-tone voice.
The presence of a contralateral hemiplegia soft palate palsy and Claude Bernard-Horner syndrome due to lesion of the X nerve, the corticospinal or pyramidal pathway and the pupillary fibers, caused by a tumor or by a vascular lesion, constitutes Avellis syndrome . Poliomyositis and dermatomyositis, due to direct involvement of the laryngeal and pharyngeal muscles, produce dysphagia and hoarseness and must be differentiated from lesions of the vagus nerve.
Pair XI or spinal nerve
Spinal nerve palsy produces alterations in the trapezius muscle and the sternocleidomastoid. The patient will not be able to shrink the affected shoulder and a slight rotation of the scapula will be observed. The sternocleidomastoid muscle will not contract firmly when attempting to move the head against the resistance of the examiner's hands to the opposite side.
The most common cause of nerve injury is whiplash. Combined spinal nerve involvement injuries can also occur in the posterior foramen.
Par XII or hypoglossal nerve
Lesions of this cranial nerve produce atrophy of the affected hemilanguage and fasciculations. As the tongue protrudes, it deviates to the affected side. When the tongue lies in the oral cavity it is slightly deviated towards the healthy side.
These injuries are rare. Poliomyelitis and systemic motor disease can affect the hypoglossal, just as Paget's disease can affect the nerve cord.
Multiple cranial nerve palsy.
There are diseases that can affect several cranial nerves. This can occur in trauma and in infectious processes such as herpes. In central lesions, on the other hand, there will be successive paralysis of the cranial nerves with late and mild changes of the long sensory and motor pathways, when the lesion affects the surface of the brainstem. When the lesion is intramedullary, the reverse phenomenon is observed.
This is how a series of multiple paralysis syndromes (from Vernet, from Collet-Sicard, from Villaret) has been described. Wallenberg syndrome, due to thrombosis of the vertebral artery or posteroinferior cerebellar artery, is characterized by affecting pairs V, IX, X and XI, with ipsilateral paralysis of these pairs, Claude Bernard-Horner syndrome, cerebellar ataxia and loss Contralateral pain and temperature sensitivity.
There are several diseases (chickenpox, rubella, measles, mumps, scarlet fever, Landry-Guillain-Barre syndrome) that can cause cranial nerve palsies along with deficits in sensation.
ABNORMAL FINDINGS ON MOTILITY SCAN
In the exploration of voluntary motility, alterations can be found, such as paralysis or plegia and paresis; paralysis is the abolition or total lack of strength, while its decrease is called paresis. Paralyzes and paresis are named according to their distribution. This is how we speak of hemiplegia or hemiparesis when a hemibody is involved; monoplegia or monoparesis if a limb is affected, paraplegia or paraparesis if the lower limbs are involved; and quadriplegia or quadraparesis if the alteration is in all four limbs. A muscle group or a specific muscle may also be affected.
Voluntary motility is carried by the corticospinal route. This pathway has two neurons, a central one, located in the posterior frontal region, and a peripheral one located in the anterior horn of the spinal cord, or in the equivalent nuclei of the brainstem of the cranial nerves. It is the corticospinal or pyramidal pathway that intersects to the opposite side at the level of the bulbar pyramids.
This pathway can be damaged centrally, in the central neuron or in its axon, giving rise to a pyramidal syndrome; while the injury of the peripheral neuron or second neuron or that of its axon will cause a peripheral motor syndrome. The lesion can be vascular, tumor, degenerative, infectious, metabolic, autoimmune, toxic, and so on.
Central motor neuron injury . The paralysis will be on the opposite side of the lesion if it occurs before the bulbar crossover, and on the same side if the lesion occurs below the decussation.
If the lesion is located above the internal capsule, the paralysis may be of the lower or upper limbs or alter sphincter movement. If the location of the lesion is cortical, the patient will present seizures and / or aphasia.
When the injury occurs at the level of the compact bundle of the internal capsule, the paralysis will be of the upper and lower limbs. If it is located at the level of the brainstem, hemiplegia is called alternate.
Weber syndrome . The lesion is at the pedicle level, a contralateral hemiplegia is observed with ipsilateral paralysis of the third common ocular motor or pair.
Millard-Gubler syndrome . The lesion is at a low pedicle level, with contralateral hemiplegia and ipsilateral superior and inferior facial paralysis.
Déjerine syndrome . The lesion affects the anterior part of the bulb, with contralateral hemiplegia and ipsilateral greater hypoglossal paralysis. If located below the pyramidal crossover, a direct spinal hemiplegia is observed.
Brown-Séquard syndrome . It is usually due to spinal hemisection due to stab wounds. An ipsilateral hemiplegia is seen with loss of deep sensation on the same side and loss of superficial sensation on the contralateral side.
If the lesion is located in the final part of the cord, a terminal cone syndrome occurs, with paralysis of the lower limbs, sphincter alterations and loss of sensation in the perineum, in a saddle.
Peripheral motor neuron injury . Peripheral motor neuron injury is associated with paralysis, fasciculations, and atrophy. The reflections are abolished.
Plexus injury . The injury to the plexuses causes a motor and sensory deficit. The motor deficit will encompass more than one motor root.
Injury to a peripheral nerve . Injury to a peripheral nerve causes paralysis and loss of sensation in the territory it innervates. The paralysis will be located in the muscle or muscles controlled by that nerve.
Other disorders of voluntary motility . Myotonia is the difficulty in relaxing voluntarily contracted muscles. It can be localized or unitaleral. It is a manifestation of muscular disease due to a primary disorder of the sarcolemma. It can be seen in myotonic dystrophy (Steinert's disease) and in congenital myotonia (Thomsen's disease).
The gravis is characterized by progressive fatigability in exercise and fatigue. It frequently affects the oculomotor, pharyngeal and laryngeal muscles, improving with rest and with cholinesterase inhibitor drugs. It is a symptom of disease of the neuromuscular synapse.
The bradykinesia is the decrease or absence of spontaneous movements along with the slowness and difficulty in voluntary movements. This trait is seen in extrapyramidal syndromes.
The apraxia is the difficulty in performing movements utility. In this alteration there are no disorders in motility or in the understanding of orders or in the recognition of objects.
In hysterical paralysis there are reflexes and there is no muscle atrophy. These facts differentiate it from organic paralyzes, in which there is atrophy and reflexes are not obtained.
| Table 32.2 Difference between lesions of the central neuron and the peripheral neuron |
|
| Central neuron | Peripheral neuron |
| Diffusely affected muscle groups | Isolated muscles |
| Initial flaccidity and then hypertonia | Hypotonia |
| Associated movements (synkinesias) | There is not |
| There is no atrophy | Atrophy |
| Increased tendon reflexes; cutaneous severely diminished or abolished | Tendon reflexes diminished or abolished; cutaneous present |
| Babinski's sign, clonus | No Babinski sign or clonus |
ABNORMAL FINDINGS ON MUSCLE TONE EXAMINATION
Alterations in muscle tone consist of decreased tone or hypotonia, and increased tone or hypertonia.
Muscle hypotonia . It is found in peripheral nerve lesions, in the initial phase of central neuron lesions, in cerebellar lesions, and in chorea.
Muscle hypertonia. It can be observed in lesions of the cerebrospinal tract, in muscular dystonias and in conditions of the extrapyramidal pathways. In the latter, the tone can be permanently increased (in a lead pipe) or temporarily, or in a cogwheel, due to its similarity to the passage on a toothed gear when passively mobilizing a patient's limb.
In persistent involuntary tonic contracture, due to trauma or inflammatory processes, and in meningitis (Kernig and Brudzinsky signs), there is also hypertonia. The Kernig and Brudzinsky signs indicate meningeal irritation of any etiology. Kernig's sign consists of flexion of the knee when attempting to flex the extended lower limb.
The Brudzinsky sign is sought with the patient in the supine position; when trying to flex the neck, flexion of the lower limbs occurs at the knees.
Tetany is a contracture of the distal muscles of the limbs, which sometimes also affects the face. Members can adopt a certain attitude, such as the midwife's hand. It is a painful contracture. It is produced by hypocalcemia of any etiology, and more rarely by hypomagnesemia.
Cramps are temporary, painful contractures, sometimes nocturnal, related to excessive exercise. They are due to an insignificant muscular disorder or to alterations in sodium, potassium, calcium or phosphorus.
The hemiplegic patient presents, in the initial phase, a flaccid paralysis of the hemibody contralateral to the lesion, which may be accompanied by a paralysis of the lower portion of the face. At first the paralysis is flaccid due to the absence of muscle tone; thus, when the paralytic limb is released, the lower or the upper one, it falls abruptly to the resting surface.
When there is paralysis of the lower portion of the face, the patient, with each exhalation, produces a movement in the affected cheek, known as the sign of the pipe smoker.
In the patient with decortication stiffness due to a destructive lesion of the corticospinal tract, near the cerebral hemispheres, the upper limbs are flexed at the wrists, elbows and fingers, the legs are extended and in internal rotation, and the feet are extended.
In decerebrate rigidity, the arms are extended pronated, with hands and fingers flexed, and the legs are extended as are the feet. It is caused by injury to the diencephalon, midbrain, pons, or metabolic disorders (hypoxia, hypoglycemia).
ABNORMAL FINDINGS IN THE TROPHISM EXPLORATION
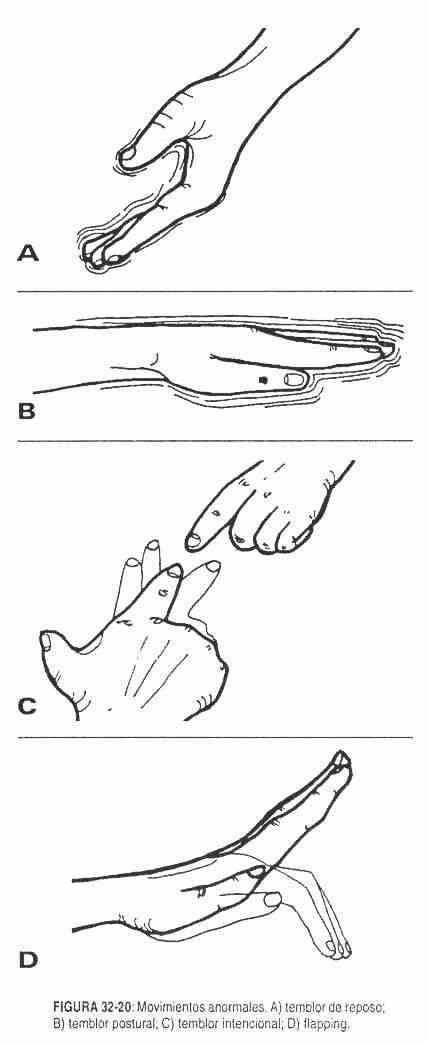 Muscle trophism depends on the normal connection of the muscle with the peripheral motor neuron.
Muscle trophism depends on the normal connection of the muscle with the peripheral motor neuron.
Its alterations include atrophy or loss of muscle mass and muscle hypertrophy.
In peripheral motor neuron lesions the atrophy is distal. Muscle atrophy also occurs in immobile muscle for a long time, as in primary myopathies.
Hypertrophy or increased muscle mass can be observed in athletic subjects and in Thomsen's disease, or myotonia congenita, where there is generalized muscle hypertrophy.
Muscle pseudohypertrophy is a condition of atrophy masked by interstitial fat.
It is recognized by muscle weakness.
Trophism alterations can be observed on the skin and on the appendages; It is possible to find bedsores or bad plantar perforation, smooth and shiny skin, anhidrosis, brittle nails and skin ulcerations. Painless arthropathies, seen in neurological conditions, such as leprosy, tabes, and syringomyelia, also represent trophism changes.
ABNORMAL MOVEMENTS AND ABNORMAL FINDINGS ON EXTRAPYRAMIDAL SYSTEM EXAMINATION
Active motility is not altered in these conditions. The most important signs are found in the alterations of the muscular cone and in the reduction of the associated movements. The face is expressionless (poker player's face) and there is a tremor at rest, muscular hypertonia, and slowness in voluntary active movements, with slow coordination and normal reflexes.
Abnormal movements may consist of: a) tremors at rest (Figure 32-20, A), which disappear with action, are slow and fine, like a coin counting, and are seen in Parkinson's disease; b) postural tremors (Figure 32-20 B), which become apparent when a certain posture is adopted, and of which the best examples are hyperthyroidism, anxiety, familial, and senile tremors; and c) intentional tremor, which increases when executing a movement and is due to cerebellar lesions (Figure 32-20 C).
If a partner had to be selected to play billiards, the patient with parkinsonian tremor would be chosen among the three types of tremors, since in action he is the one who best executes the movements.
On certain occasions, when fixing the forearms, the trembling, rhythmic and progressive descent of the hands can be observed. It is called asterixis (Figure 32-20 D). It is seen in liver, kidney and lung failure. It could be called a sign of goodbye or farewell.
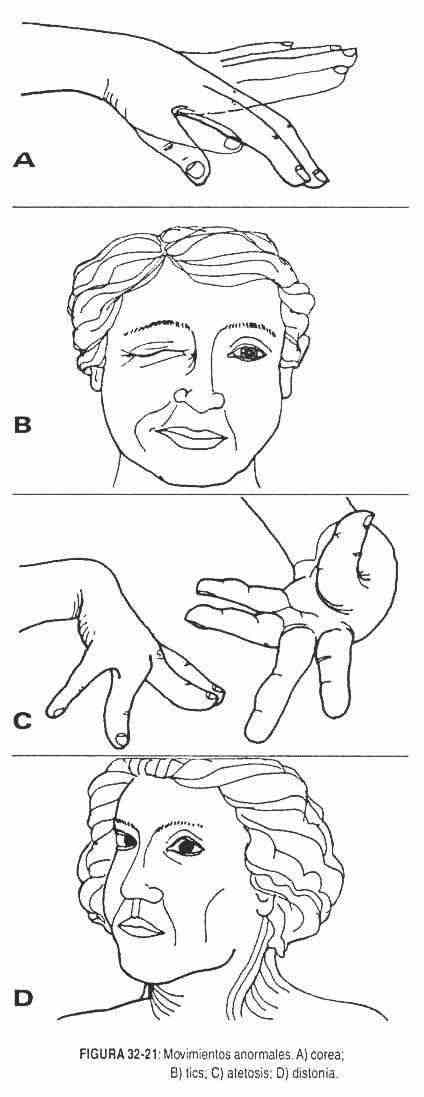 The patient may present sudden, distal, untimely movements that do not repeat themselves. They are observed on the face and upper or lower limbs, when the subject is moving or at rest, and are accompanied by hypotonia. These are the so-called choreic movements (Figure 32-21, A). They can be acute onset, as in Sydenham's chorea or rheumatic fever, or chronic onset, as in Huntington's chorea.
The patient may present sudden, distal, untimely movements that do not repeat themselves. They are observed on the face and upper or lower limbs, when the subject is moving or at rest, and are accompanied by hypotonia. These are the so-called choreic movements (Figure 32-21, A). They can be acute onset, as in Sydenham's chorea or rheumatic fever, or chronic onset, as in Huntington's chorea.
Other times, slow, crawling movements, called athetosis (Figure 32-21, C), occur on a spasmodic background on the face, neck, and trunk. They occur in hepatolenticular degeneration or Wilson's disease.
The movements similar to the choreicos, but of greater intensity and violence, are called ballistic . They occur in the proximal part of the limbs, shaking the whole body, and are produced by injury to Luys' body or its pathways.
The dystonias are similar to athetosis, and occur in large segments of the body in both axial and proximal muscles. These patients adopt abnormal positions. They are produced by the action of drugs (phenothiazines) and in the course of certain heredofamilial diseases (Figure 32-21, D).
The myoclonus are sudden muscle twitches, irregular and asymmetrical short - lived, occurring at sensitive and sensory stimuli. They occur on some occasions, normally, when falling asleep, or as an epileptic manifestation or in relation to degenerative diseases.
The tics are involuntary movements, irregular, stereotyped, inevitable for the patient and reproducing normal movements. They can be suppressed by the will for a short time (Figure 32-21, B).
The twitches are worm - like movements produced by muscle tremulación, seen through the skin. They appear due to motor neuron injury.
The facial dyskinesias are bizarre, repetitive movements bula movement Mandi, lips and tongue. They are seen in elderly, toothless, and psychotic individuals.
ABNORMAL FINDINGS IN THE COORDINATION EXPLORATION
Voluntary movements are carried out harmoniously and with precision, both in gait and in static position. This coordination is regulated by the deep sensation, the labyrinth and the cerebellum; sight also contributes to maintaining balance. The lack of coordination or its disturbances is called ataxia.
Coordination disturbances observed in gait, when the patient is instructed to walk around the room, may be labyrinthine, cerebellar, or sensory in origin.
The labyrinthine gait is the aforementioned Babinski star gait, in which the patient deviates to the same side, with a tendency to fall.
The cerebellar gait is an insecure and oscillating gait, similar to that of a drunk; the base of support is wide and it is difficult to turn.
During gait, the patient with alterations in deep sensitivity projects the foot forward, striking the heel and highlighting the insensitivity of the base that supports it. Look at the floor to make sure of its location.
The changes observed in the Romberg test may be due to labyrinthine or cerebellar disease. The patient with labyrinthine ataxia, standing up and closing the eyes, begins to oscillate and always falls to the same side. Oscillations start slowly and increase progressively. As for the patient with cerebellar ataxia, it is difficult to get them to stand with their feet together, with their eyes open or closed. In turn, when ataxia is due to a loss of positional sensitivity, the individual correctly maintains the standing position and falls when ordered to close the eyes.
The alterations observed in the heel-knee and arm coordination tests may manifest themselves in their rhythm, speed, smoothness and security, remembering that the dominant hand or leg is more precise. The patient with cerebellar lesions presents sudden movements, jumping, clumsy, without rhythm, especially when the direction of movement changes. When there is insecurity in the coordination of movements when closing the eyes, the disorder may originate in positional sensitivity. Repeated and permanent deviation to one side, worse with closed eyes, suggests vestibular or cerebellar disease.
Coarse sensory injuries, severe motor injuries, and extrapyramidal injuries can produce impaired rapid coordination movements.
ABNORMAL FINDINGS ON THE EXPLORATION OF THE REFLEXES
Cutaneomucosal reflexes and tendon reflexes can be increased or decreased or abolished. Pathological reflexes may also appear.
Reflexes can be universally or localized (hyperreflexia); when hyperreflexia is localized, the recognition is based, fundamentally, on the comparison with the opposite side. A 3+ reflex is sharper than normal and does not always indicate disease; if it reaches 4+ it is often pathological, especially when there is increased muscle tone and is associated with Babinski's sign and clonus. Hyperreflexia suggests injury to the corticospinal pathway. Hyperthyroidism can have heightened reflexes.
Diminished reflexes or hyporeflexia are not easy to assess; much more significant is the finding of areflexia. Areflexia is the lack of reflexes, confirmed after having exhausted all the distraction techniques recommended in Chapter 13. Hyporeflexia and areflexia indicate loss of the reflex arc, due to compromised sensitivity, damage to the spinal motor neuron or injury of the referring or motor branch. Muscle diseases can also cause hiccups or areflexia. Cutaneomucosal reflexes are diminished or abolished in both central motor neuron and peripheral motor neuron lesions.
The Babinski sign, clonus, kissing or snuffling and "grasping" constitute pathological reflexes, which are generally of the flexor type.
The Babinski sign consists of the extension of the first toe and the fan opening of the rest of the toes when the sole of the foot is stimulated from back to front, following its outer edge. It is of normal appearance in the children of up to 2 years; its posterior presence indicates a lesion in the corticospinal tract. This same reflex can be obtained by stimulating the anterior crest of the tibia, the Achilles tendon, or by compressing the posterior muscle mass of the leg.
It can occur in patients intoxicated by alcohol or drugs, or after a seizure.
Abrupt stretching of the Achilles tendon, produced by repeated and rapid passive dorsiflexion of the foot, or abrupt stretching of the quadriceps by pulling the patella down, can produce jerky, repetitive movements at the foot or patella level, respectively, of rapid extinction. These jerks are called clonus , which together with Babinski's sign and hyperreflexia are the characteristic findings of pyramidal syndrome.
The necking or snout and the "grasping" are normal reflexes in children. Its later finding is pathological. When stimulating the chin, the patient can make snuffling or kissing movements, while when stimulating the patient's palm, the patient may want to grasp the examiner's hand (grasping). By stimulating the fingertips or the palm of the patient's hand, movements in the chin can be observed. All of these findings are signs of frontal release from diffuse brain injury.
The "doll eyes" are a normal movement that occurs in the eyes when flexing or extending or rotating the head in the opposite direction of movement. In a patient in a coma, the loss of this eye movement suggests a lesion at the level of the pons or midbrain.
The inversion of the reflections consists in obtaining a response opposite to that expected when performing the reflections. Thus, the Babinski sign is an inverse reflex to the normal plantar flexor response; or looking for the Achilles reflex results in a dorsiflexion of the foot, rather than its extension. They occur due to injury to the reflex center, which allows, due to greater stimulation and central diffusion, the triggering of reflexes with an undamaged arch.
ABNORMAL FINDINGS ON SENSITIVITY EXAM
Sensitivity is divided, for study, into special sensitivity (sense organs), general, superficial and deep, and visceral.
The abnormal findings of special sensitivity have already been described with the corresponding cranial nerves.
Abnormal findings of general sensitivity can be objective or subjective. The subjective ones are constituted by pain, paresthesias, dysesthesias and causalgias. Paresthesias are an unpleasant sensation in the territory of the affected nerve, generally distal, similar to tingling and pricking, which when they acquire an eminently unpleasant character are called dysesthesias. Causalgia is a burning sensation, which can occur spontaneously or by tactile stimulation.
Objectively, a decrease in sensitivity or hypoesthesia and the absence of sensitivity or anesthesia are described. If it refers to pain, it is called hypoalgesia and analgesia. The increased sensitivity is called hyperesthesia; When a stimulus produces exaggerated pain, it is called hyperpathy.
Loss of all sensation in the distribution area of a peripheral nerve occurs in lesions of that peripheral nerve. When there is a lesion in the sensory root, in turn, all sensations are lost in one or more dermatomes. Loss of pain and thermal sensitivity occurs in one or more dermatomes when there is a spinal cord injury, as seen for example in syringomyelia. Loss of sensitivity to vibratory, positional, two-point separation, and stereognostic pressure occurs below the level of the lesion and on the same side, in Goll and Burdach bundle or posterior spinal column conditions.
Loss of sensation with spontaneous onset of pain on the opposite side of the injury can be seen in thalamic lesions, while loss of sensation of two-point separation on the opposite side of the injury occurs in certain sensory cortex lesions.
ABNORMAL FINDINGS IN THE EXPLORATION OF THE LANGUAGE
Oral language abnormalities include dysarthria, aphasia or dysphasia, aphonia or dysphonia, palatal palsy, cerebellar dysarthria, and the word Parkinsonian syndrome.
Dysarthria is a defect in the articulation of the word that is produced by a motor deficit in the lips, tongue, palate or pharynx. Aphasia or dysphasia is a defect in the creation of the word or in the strength of its expression. It occurs in patients with damage to the cortical centers of the word. There may be errors in the choice of words or syllables, dysphasia, or a total disability for language: aphasia. These patients have normal motor function of the mouth and larynx.
Dysphonia or aphonia is a defect in the volume or quality or tone of the voice. It occurs in patients with laryngeal disease.
Cerebellar dysarthria is an uncoordinated, irregular word, with separation of the syllables.
The word of the patient with palatal palsy is uttered in a nasal voice; while the speech of the patient with Parkinson's disease is slow, tired, as in a whisper.