by Alberto J. Muniagurria and Eduardo Baravalle
LIPS
The function of the lips in speech, ingestion, control of salivary secretion and in mimicry is governed by the orbicularis muscle. Because they cover the hard structure of the teeth, they are easily damaged. Congenital alterations of the shape, color, size, surface, moisture, and added lesions are described regarding the abnormalities of the lips.
The lips can be deformed from birth, as occurs in cleft lip, which is due to the lack of union of the nasolabial folds during fetal life. The defect can affect one or both sides of the upper lip, extend down the floor of the nose through the gums and roof of the mouth, and even be complete on its way to the pharynx.
Macrocheilia, or large lips, is seen in patients with hemangiomas and lymphangiomas. They are more common on the upper lip.
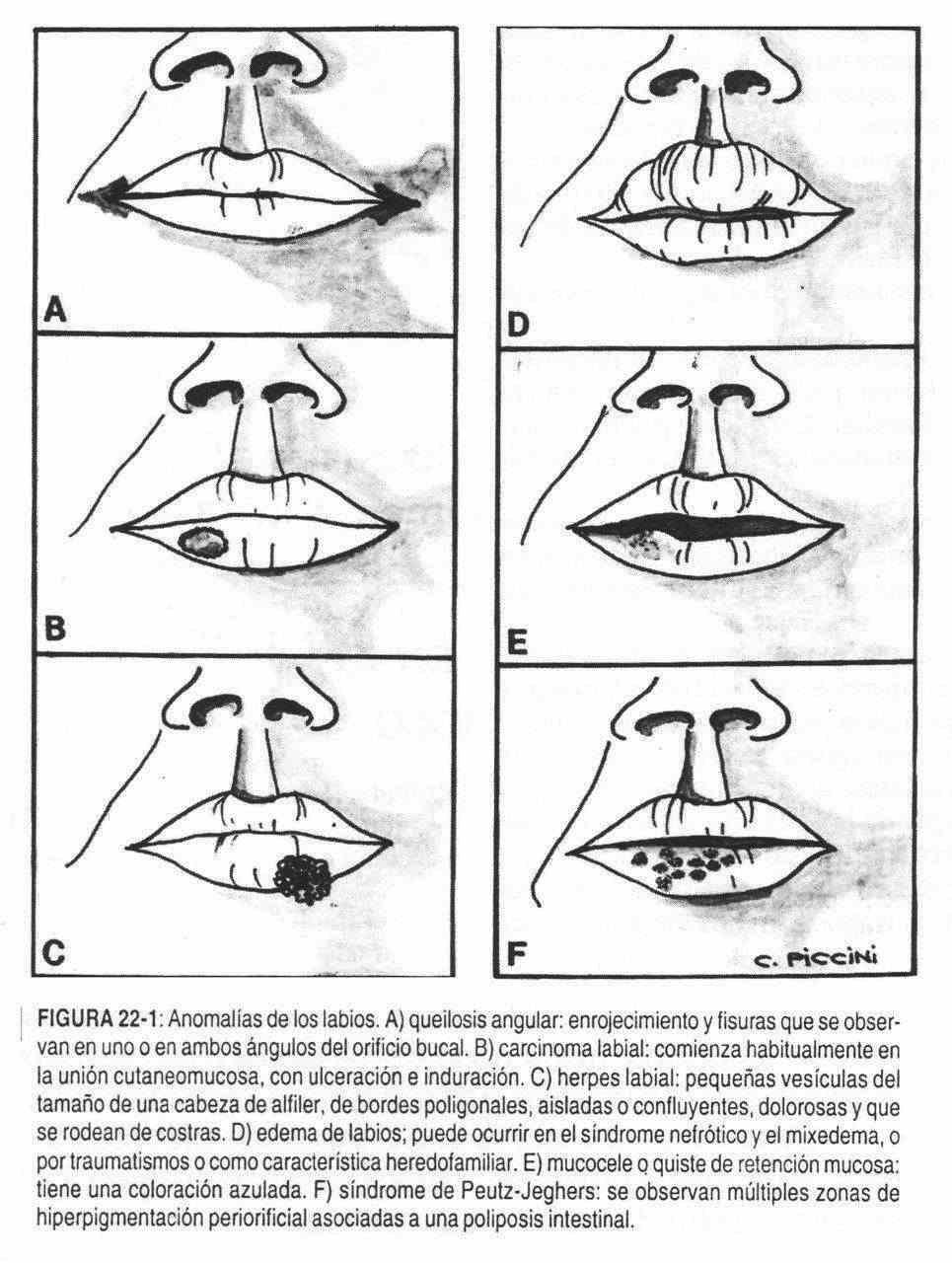
In cases with generalized edema, the lips may become swollen, as in nephrotic or myxedematous patients (Figure 22-1, D); or they may be part of more localized conditions, such as Quincke's edema and hereditary family edema. The lips can be extremely dry, as occurs in feverish patients or patients with diabetes mellitus or severe dehydration of any etiology.
The cold sore, or simple, or fire, is a common infection that begins with small, transparent, pinhead-sized vesicles surrounded by a red, painful halo that quickly turn into scabs (Figure 22-1 , C). This rash can spread to the nose and cheeks.
Heavy smokers may have white, plaque lesions frequently located on the lower lips, called leukoplakia. Also, in elderly individuals with keratosis with induration and ulceration, the possibility of squamous cell carcinoma that begins at the cutaneomucosal junction should be suspected (Figure 22-1, B) and is common on the lower lip and in humans. It can also be seen as a nodule with satellite adenopathy. It is possible that a painless, black or brown, or discolored, sometimes ulcerated lesion that constitutes a melanoma may appear at the level of the lips or anywhere in the mouth.
Other times, a rounded, regular, bluish, or translucent mass is seen, called a mucocele or a mucous retention cyst (Figure 22-1, E); it is a benign lesion of fundamentally aesthetic importance.
The lower lip can be the seat of a chancre, the existence of which should be suspected in a patient suffering from a painless, persistent and firmly indurated lesion. Adults who, as children, have suffered from congenital syphilis, frequently present fine scar lines that start from the mouth run through the lips and cheeks. They are the fast calls.
Maculopapular lesions, ulcerated or not, are occasionally seen as part of secondary syphilis. Tertiary syphilis presents with rubbery lesions that can lead to ulceration of the tongue, palate, or lips. Orogenital sexual practices can cause gonococcal lesions on the lips, tonsils, tongue, and pharynx.
In riboflavin deficiencies, it is not unusual to observe the existence of lip clefts (Figure 22-1, A); the most frequent cheilitis are caused by vitamin deficiency. Infection of the corner of the mouth by monilias, or perleche, produces thickening and desquamation of the epithelium in the corners of the mouth, giving rise to the appearance of fissures (cheilosis). These injuries are seen mainly in children, but can also affect adults. Similar lesions can appear when, due to the existence of bad teeth, saliva drains towards the corners, producing ulceration of the skin.
In discoid lupus, when it affects the lips, a depigmented area is observed, with a hyperpigmented margin. On the lips it is also possible to appreciate the bluish color of cyanotic patients, or the brownish-gray color of patients with adrenal insufficiency.
In the lips, there are also alterations of the blood vessels. For example, small blue dots or varicose veins, or small raised, strawberry-colored nodules that are hemangiomas or lymphangioma. In Rendu-Weber-Osler disease, small red angiomas are seen, located subcutaneously. In Peutz-Jeghers syndrome (Figure 22-1, F), pigmented spots or dots are seen on the oral surface of the lips and cheeks, associated with intestinal polyposis.
Gums and teeth
 The teeth and gums can be the seat of manifestations of systemic diseases, and their condition can also affect the health of the patient. The gums can present infectious, inflammatory and tumor lesions and can also alter their color in different diseases.
The teeth and gums can be the seat of manifestations of systemic diseases, and their condition can also affect the health of the patient. The gums can present infectious, inflammatory and tumor lesions and can also alter their color in different diseases.
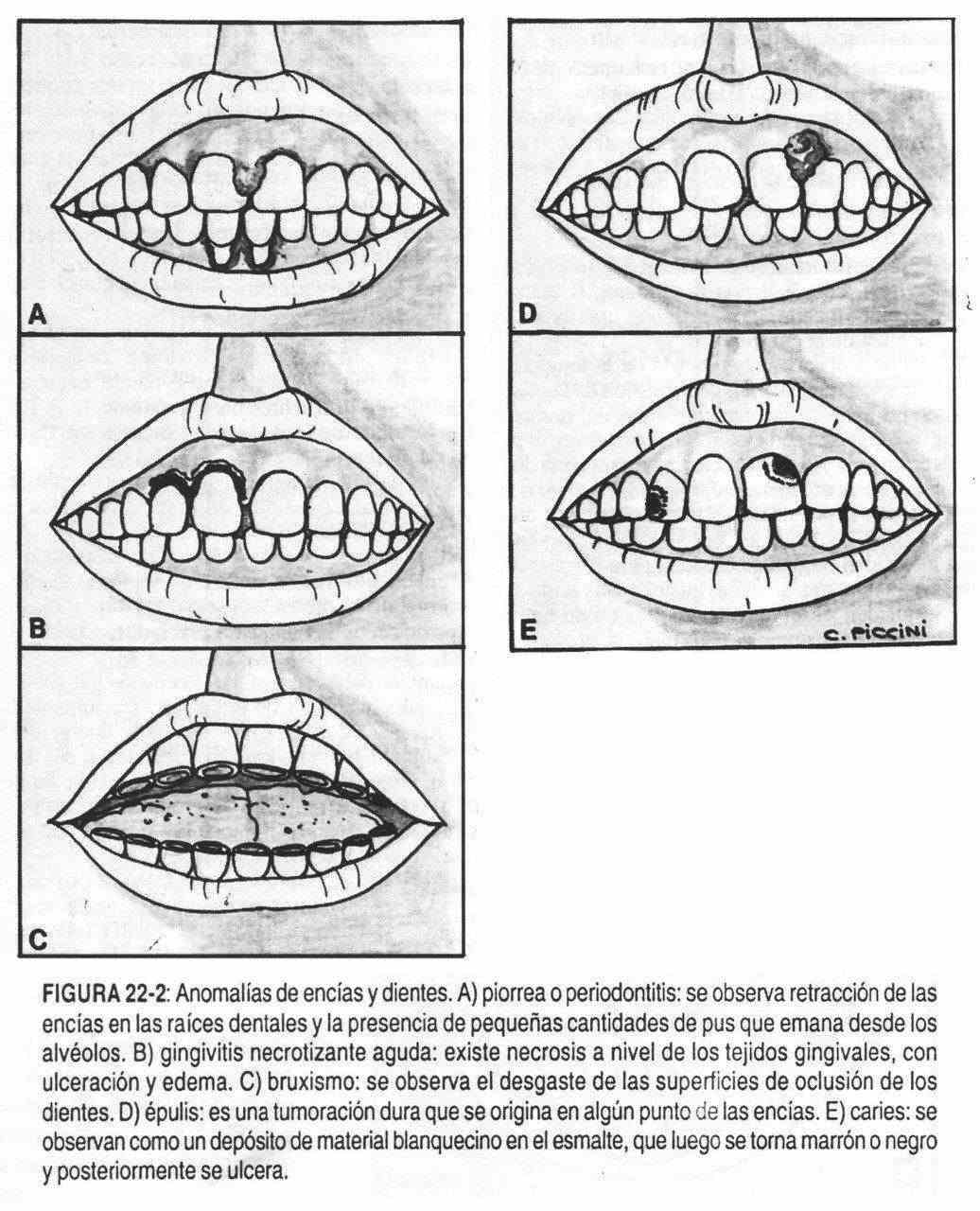
Alveolar pyorrhea (Figure 22-2, A) (Riggs disease) is characterized by retraction of the gums from the tooth roots and the presence of small amounts of pus draining from the alveoli. In older people this disease leads to the loss of teeth.
Inflammation of the gums characterized by redness, swelling, pain, and ulceration of the gingival tissues is known as acute necrotizing gingivitis or trench mouth or Vincent's stomatitis (Figure 22-2, B). In addition, ulceration of the interdental papillae and grayish membranes can be seen on the inflamed and ulcerated edges.
Although rare in frequency, the gums can also give rise to tumors. Fibromas, which appear in patients with tuberous sclerosis, or isolated formations, are seen as a hard tumor at the gingival margin, joined by a narrow pedicle, called epulis (Figure 22-2, D), a giant cell tumor It is caused by an inflammatory reaction. Both epulis and fibroids are benign tumors. The gums can also be affected in von Recklinghausen neurofibromatosis, leading to the appearance of the characteristic tumors of this disease.
In lead poisoning, the lead line or Burton's line is observed, characterized by being a finely dotted black or grayish line, which is found on the gum just below where the tooth emerges or on the border between tooth and gum. Other heavy metal poisonings, especially bismuth, can be the cause of a similar line.
Chronic mercury poisoning produces spongy gums, with loss of teeth. A brown-blue-gray spot-like line is seen in adrenal insufficiency (Addison's disease). This pigmentation is normal in black subjects and in subjects with dark skin, and also, occasionally, in people with light skin.
In vitamin C deficiency, or scurvy, the gums may be soft, sore, spongy, and bleeding; in these cases the teeth can be extracted with the fingers. In gingival hypertrophy or enlargement, the gums partially cover the teeth, which is seen at puberty, in pregnancy, during treatment with hydantoins, and in acute monocytic leukemia.
The presence of ecchymotic spots on the gums should make one suspect the existence of hemorrhagic diseases.
The teeth may be altered in their quantity by previous extractions, or present cavities, or have alterations in their shape or color. The examination should also observe the mandibular occlusion and the parotid duct orifice.
Anodontia or lack of teeth is a rare entity, there are family cases. The case of children with double dental rows is equally exceptional.
Tooth decay, a common tooth condition, is first seen as a deposit of white plaster on the enamel surface of the teeth, and then as a brown or black white cavity (Figure 22-2, E). They are often not seen with the naked eye and special dental techniques are necessary, including X-rays.
The permanent teeth, or more frequently the upper central incisors, may be clipped at the cutting surfaces, be smaller and further apart, with their sides narrower. They are the so-called Hutchinson teeth that make up, together with interstitial keratitis and labyrinthine disease, the Hutchinson triad, characteristic of congenital syphilis. Here the affected teeth are the permanent ones, and not the accessories. Screwdriver teeth can also be seen in congenital syphilis, as can macro and microdontism.
The presence of excess fluoride in drinking water produces a yellowish, brown or black coloration on the teeth, giving rise to the appearance of the characteristic teeth of fluorosis or mottled enamel (south of Córdoba, Río Cuarto and south of Buenos Aires ).
An earthy substance, called tartar, produced by microorganisms and alkaline salts (bacterial plaques) can accumulate on the gingivodental line.
In bruxism, scraping or grinding movements made during sleep or unconsciously in wakefulness, the occluding surfaces of the teeth appear worn (Figure 22-2, C).
We must also evaluate mandibular occlusion. A malocclusion can indicate, dislocation, fractures of the jaws or of the face; both are frequently the result of a congenital or developmental abnormality. A sudden alteration in the occlusion of the maxilla will cause pain in the temporomandibular joint, and can also be the cause of headaches (Costen syndrome).
The parotid canal orifice, or Stenon's orifice, is located in the mucosa of the cheek in front of the second molar. It may be inflamed, as occurs, for example, in urban fever or mumps. It is around this orifice that we also find Koplick's spots, white, rounded, with a small erythematous halo, characteristic of measles. It is also possible to observe yellowish granules, or Fordyce spots, which correspond to sebaceous glands.
LANGUAGE
 The careful examination of the tongue is a practice that has been carried out since the early days of medicine and that can provide signs that help diagnose the disease.
The careful examination of the tongue is a practice that has been carried out since the early days of medicine and that can provide signs that help diagnose the disease.
We must observe the symmetry of the tongue and the muscular coordination in its protrusion, as well as the characteristics of the lingual dorsum; in addition, retract it laterally to see its back and the floor of the mouth. It is in this area where malignant diseases frequently settle. We will order the patient to touch the palate with the tip of the tongue to see its ventral surface. Tongue mobility is essential for various functions: speech, chewing, taste, and salivation.
Alterations in its size, color and shape, changes in the papillae, presence of venous, tumor and erosive lesions, motility and abnormal movements can be observed, and the normal humidity of the oral cavity may be lacking.
Large tongue or macroglossia can be seen in hypothyroidism, Down syndrome, acromegaly, or in inflammatory, cystic, or neoplastic diseases. Asymmetries caused by neurofibromas, hemangiomas or lymphangiomas, and amyloidosis can also be seen.
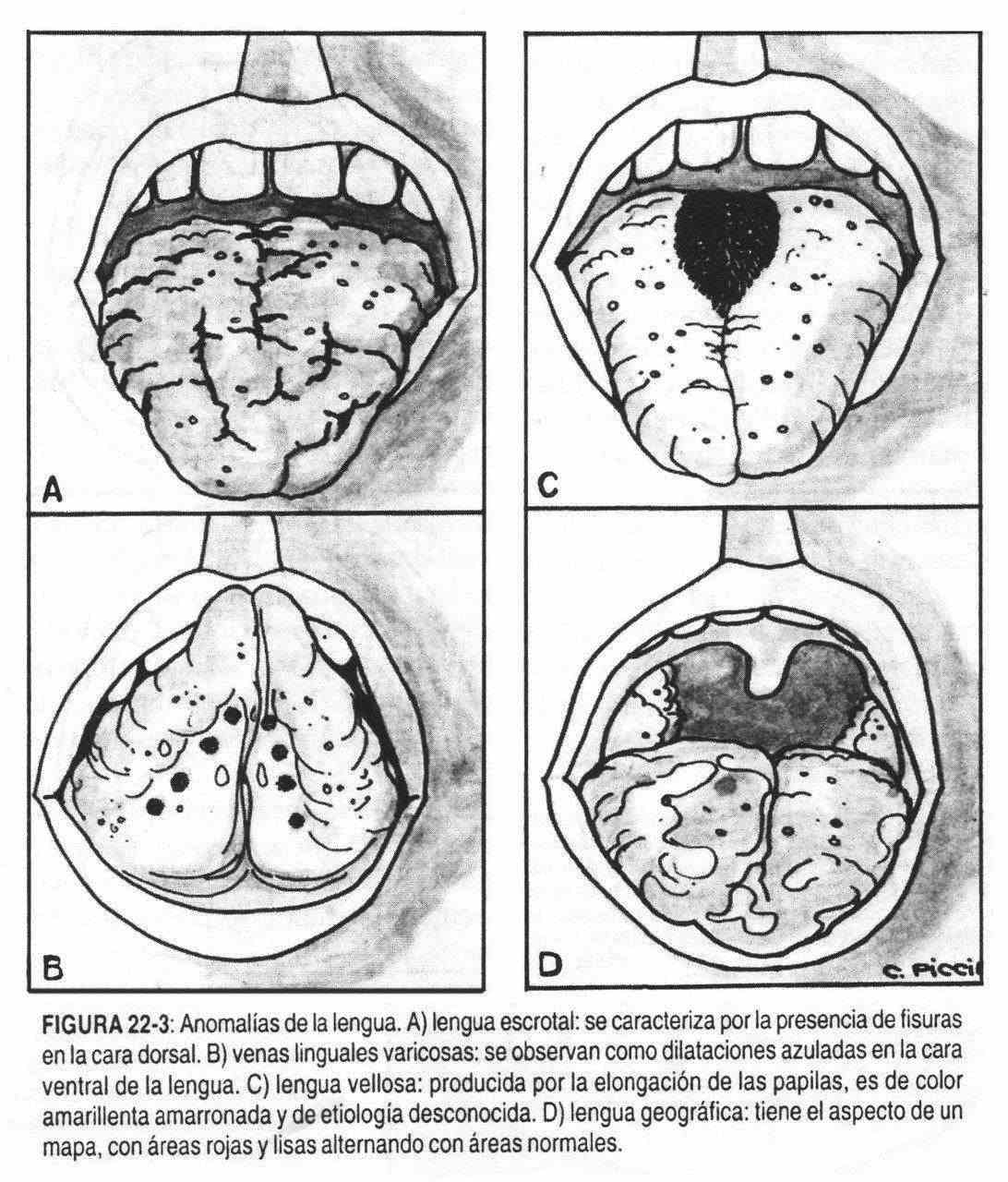
The red tongue without papillae, a process that usually begins at the edges, suggests a deficiency of vitamin B12, niacin or iron and constitutes the so-called smooth tongue. In contrast, when the papillae are elongated, brownish in color, they constitute the so-called hairy tongue (Figure 22-3, C), clinically benign, of unknown etiology, which alarms and bothers the patient.
Fissures can appear in the tongue with age and be very numerous, giving rise to the appearance of the scrotal tongue (Figure 22-3, A), which is sometimes associated with vitamin B deficiency and improves with this complex . The geographic tongue, alarming in appearance, is characterized by red and smooth areas alternating with normal areas, giving the appearance of a map that changes over time (Figure 22-3, D). This alteration is benign and of unknown cause.
The coated tongue is a whitish tongue, which is produced by lack of the natural desquamation of the lingual epithelium; it is generally found in patients who do not eat food by mouth. Other times there are thickened, white plaques adhering to the mucosa, with the appearance of white paint. They are the so-called leukoplastic lesions, whose meaning is variable; they are frequently seen in smokers and may constitute premalignant lesions.
In some infectious diseases the tongue has a characteristic appearance. In typhoid fever it is wrinkled and covered with brown sores. In scarlet fever it may be red, with enlarged and reddened papillae, slightly coated, giving rise to the so-called fruity tongue, which contrasts with the periorbital paleness. Other times it is possible to observe the presence of a white, soft, velvety-looking crust called thrush, caused by an infection by Candida albicans. It is common in children and immunosuppressed patients.
In other entities, a pale, smooth, shiny, and atrophic tongue is seen, as in pernicious anemia, Plummer-Vincent syndrome, and sprue. In the early stages of pernicious anemia, despite being inflamed, it may appear normal. Also in some cases of sprue it is seen red, inflamed and Asurada. In pellagra, it first has a rough and edematous appearance, and later it becomes soft and intensely red with signs of glossitis. In smokers there may be a certain degree of glossitis with brown or grayish spots. Sometimes in Addison's disease, the tongue has irregular, round or oval spots with brown or black pigmentation. Antimalarials, contraceptives and tranquilizers can cause hyperpigmentation of the oral and lingual mucosa.
Small blue or purple bumps called by their appearance "caviar lesions" may appear on the ventral surface of the tongue. These are lingual vein varices (Figure 22-3, B) and are devoid of pathologic value. The observation of a tense cyst on the floor of the mouth, under the tongue and next to the molars, is due to an obstructed sublingual gland. The cyst is usually single and filled with a thick, clear, mucous fluid.
Paroxysmal coughing fits and fits of whooping cough cause protrusion of the tongue; As a result, the frenulum is constantly traumatized against the edges of the incisors and erosions or ulcers can occur. Sublingual ulcers also occasionally appear in histoplasmosis. In tuberculosis, an ulcer with indurated edges is sometimes observed, with an exudative background, while in actinomycosis there may be a yellowish discharge, located anywhere in the oral cavity.
Canker sores are small, painful ulcers with an inflamed base and deep crater, usually found on the lingual borders. These ulcers can be multiple and affect the tongue, the jugal mucosa, the palate or the floor of the mouth. In Beh ^ et syndrome, canker sores are seen in the mouth, eyes, genitals, and skin, along with manifestations in the central nervous system and in the digestive tract.
 We can also observe scars on the tongue, common in epileptics who during seizures have suffered bites from their tongue.
We can also observe scars on the tongue, common in epileptics who during seizures have suffered bites from their tongue.
Accompanying dermatological lesions, pemphigus can manifest in the oral cavity by bullous and vesicular lesions, as can erythema multiforme and Stevens-Johnson syndrome. Erosions that are indurated and that do not heal quickly should raise the suspicion of a neoplasm.
The submaxillary gland can be enlarged by destructive, inflammatory or tumor processes. Its exit orifice should be observed on the floor of the mouth, and the presence or absence of pain and peripheral lymphadenopathy, which will orient towards obstructive, inflammatory and neoplastic processes, respectively.
In lesions of the central nervous system that affect the nucleus of the twelfth nerve, or the greater hypoglossal nerve, the tongue does not protrude in the midline and deviates to the injured side. Rhythmic protrusion and retraction movements can be seen in Parkinson's disease, and athetoid movements in patients with cerebral palsy along with excessive salivation. In myasthenia gravis, the tongue shows extreme fatigue, as occurs in the eyelids and other voluntary muscles. Dryness of the oral mucosa and the absence of the normal amount of saliva on the floor of the oral cavity can be observed in severe dehydration, after radiation therapy, and in xerostomia or Sjogren's syndrome.
OROPHARINGE
Regarding changes in the oropharynx, changes in color and shape, the presence of plaques and / or exudates, and the existence of tumors should be described.
The general redness of the throat or pharynx indicates the existence of a pharyngeal congestion or pharyngitis, or the first stage of a scarlet fever or diphtheria, or some other infectious process of various etiology. Smoking patients present diffuse redness of the oral mucosa and pharynx.
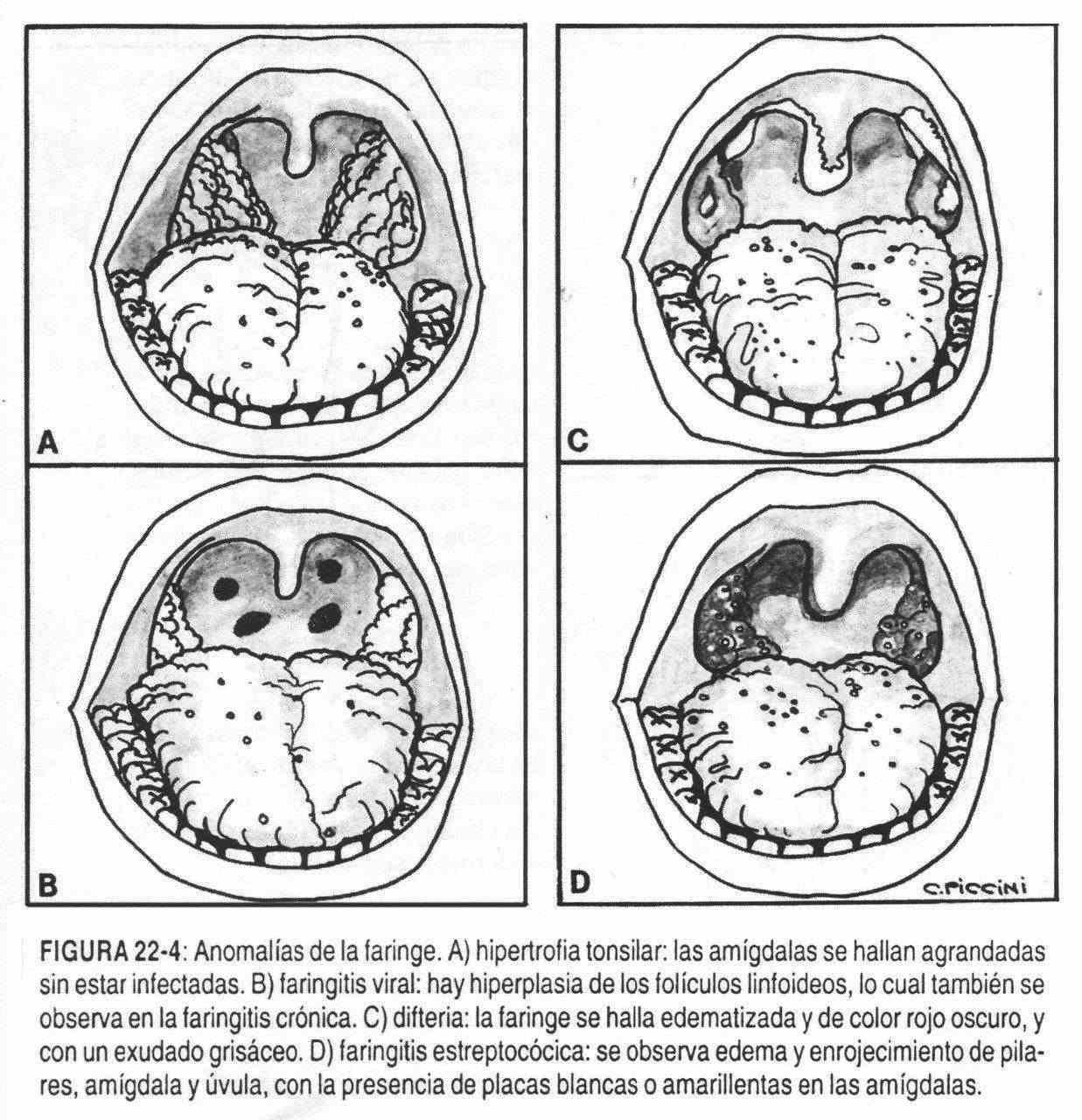
Classically streptococcal infection causes swelling and redness of the tonsils (Figure 22-4, D), pillars, and uvula with the addition of white or yellow plaques. Diphtheria (Figure 22-4, C), currently rare, is characterized by a dark, swollen throat, with the formation of a firm, grayish exudate, which can spread over the soft palate and uvula; removal of exudate leaves a bleeding surface. The mucous membranes of the oral cavity, sometimes including the tongue, are part of Plummer-Vinson syndrome (dysphagia, iron deficiency anemia, and mucous membranes). When the inflammation of the pharynx takes on gangrenous-necrotizing characteristics due to the action of anaerobic germs, it is called Vincent's angina. In viral pharyngitis (Figure 22-4,
A pharyngeal redness with or without hemorrhagic phenomena at the level of the gums can be part of the clinical picture of hemorrhagic fever, whereas the Coxsackie A viruses give rise to painful vesicles in the oropharynx, which ulcerate and are accompanied by lesions in the palms and soles; constitute the so-called disease of the mouth, palms and soles.
When the infection is caused by an adenovirus, it is usually accompanied by conjunctivitis. Parainfluenza viruses can cause pharyngitis, but are mainly characterized by rhinitis or coryza. Infectious mononucleosis produces a painful tonsillar and peritonsillar inflammation with a thick whitish exudate, whereas in candidiasis there is a whitish exudate at the level of the pillars, pharynx and tongue.
In hematologic diseases (leukosis, thrombopenias, and leukopenias), hemorrhages and ulcerations of the pharynx, soft palate, gums, tongue, and uvula may be seen. Lymphomas can present tonsillar lesions. In chronic pharyngitis, a reddening of the pharynx is also observed, along with mucosal shedding and hyperplasia of the lymphoid follicles.
Tumors, benign and malignant, can develop on the hard and soft palate. The so-called torus palatinus is a hard tumor, of the midline, of bony appearance, benign, but that interferes with the function of the palate. The bony palate and the soft palate can give rise to a mixed tumor of the accessory salivary glands that is manifested by a moderately hard and rounded mass. Malignant tumors of the palate are rare in frequency and present with ulcerated masses or nodules. Among tobacco chewers, especially in Southeast Asia, who commonly chew a mixture of walnuts, slaked lime, and tobacco, ulcerated lesions may appear, fixed to the jaw, constituting carcinoma of the gingivojugal sulcus.
Palatal perforation was, in the past, almost exclusive to syphilis, but today it is seen in patients with carcinoma or who have received radiation therapy. In some cases, the perforation can be congenital. In Marfan syndrome and Turner syndrome, a high arched palate is seen.
The oropharynx, nasopharynx, and hypopharynx can be palpated. To do this, the patient with his mouth open, the tongue will be held with gauze. The gloved finger can be gently and carefully explored in all directions, including the top and back of the soft palate. This is how retropharyngeal abscesses can be palpated in children with vertebral tuberculosis. These children will have a peculiar cough that the French call "cri du canard" (duck cry).
Some patients with peritonsillar abscesses may present with an inability to open their mouth, a stiff neck, and fever, symptoms that can lead to a false diagnosis of tetanus. Due to the impossibility of opening the mouth, a good digital palpation of the oral cavity, if possible, is necessary in these patients with oral disease.
Sometimes a bifid uvula is seen within the palatoschisis, which usually includes a nasal voice. Bifid uvula can produce an irritating cough, more intense at night, because the decubitus allows the uvula to rest on the base of the tongue. Other times, in patients with aortic regurgitation, a beat synchronous with the heart beat is seen in the uvula. Inflammation of the uvula and soft palate the day after a copious alcohol intake is common.
PAROTIDA
Located in front and below the ear, and extending from the masseter muscle to the sternocleidomastoid muscle, it can be the seat of different diseases that cause enlargement of the gland. This enlargement can be acute or chronic. Among the former, infectious causes, especially the urban fever virus, in addition to calculi, mucous plugs of the Stenon duct, and traumatic causes deserve to be mentioned. Chronic enlargements are more varied and include: lead poisoning, Sjogren's syndrome, lymphomas, leukemic infiltrations, solid tumors of the parotid, alcoholism, diabetes, sarcoidosis, and actinomycosis.
TEMPOROMANDIBULAR JOINT
This joint may have anterior and posterior subluxations. It can also be affected in cases of osteoarthritis and less frequently in rheumatoid arthritis. The disease that most commonly affects this joint is myofacial pain syndrome, characterized by facial pain and mandibular dysfunction without clinical or radiological evidence of organic damage. The nuclear magnetic resonance study is the one that defines the subluxation.