by Alberto J. Muniagurria and Eduardo Baravalle
ALTERATIONS IN THE ARTERIAL PULSE
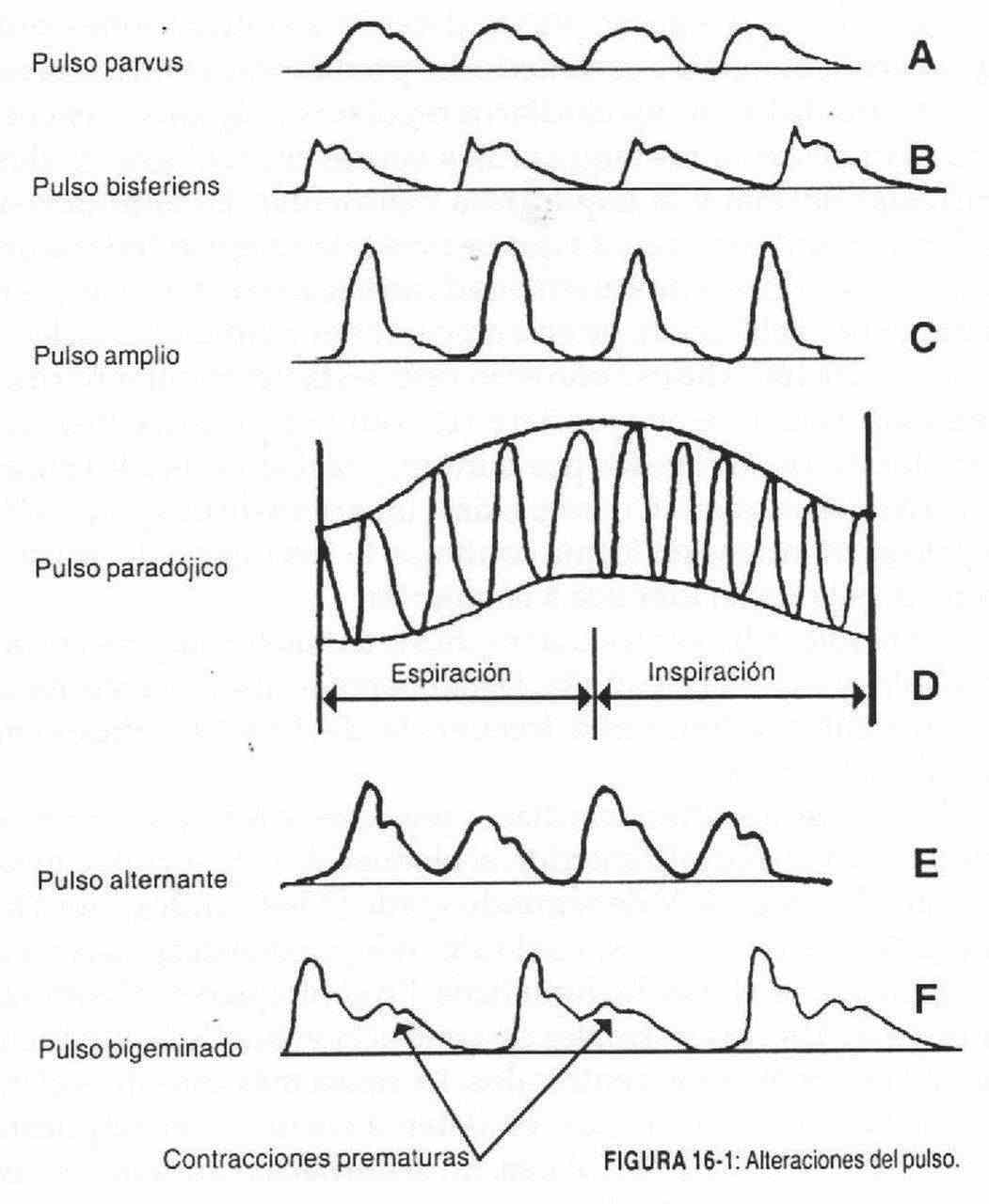 The arterial pulse can be abnormal due to alterations in rate, rhythm, shape, amplitude, and tension. The study of these qualities can provide valuable data on left ventricular ejection. The search for abnormal arterial pulse findings is usually done by evaluating the radial pulse; in its absence abnormalities can be sought in the carotid pulse. The pulse should be taken for sixty seconds, especially if it is irregular. The arterial pulse may be absent if the palpated artery has been previously catheterized.
The arterial pulse can be abnormal due to alterations in rate, rhythm, shape, amplitude, and tension. The study of these qualities can provide valuable data on left ventricular ejection. The search for abnormal arterial pulse findings is usually done by evaluating the radial pulse; in its absence abnormalities can be sought in the carotid pulse. The pulse should be taken for sixty seconds, especially if it is irregular. The arterial pulse may be absent if the palpated artery has been previously catheterized.
Frequency alterations . When the arterial pulse has a frequency less than 60 beats, it is called bradysphigmia, and when it has more than 100 it is called tachysphigmia.
It should not be taken at the pulse rate as an index of the heart rate. Sinus tachycardia (100-150 beats / min) is a rhythm that originates in the sinus node and is conducted through normal routes, and can constitute a normal response to exercise, anxiety, hyperthyroidism, anemia or fever, or being a compensation mechanism against a decrease in cardiac output. Sinus bradycardia (50-60 beats / min) is of sinus origin and conduction is normal in it. It is commonly seen in trained individuals and in hypothyroidism, sinus sinus syndrome, second-degree atrioventricular (AV) block, and complete AV block, and with the use of drugs such as amiodarone and beta-blockers.
Rhythm disturbances . In normal conditions the rhythm should be regular. Also in these conditions, isolated extrasystoles or premature ventricular contractions may appear.
The variations of the rhythm can be of regular, irregular and regular-irregular type; this last pulse, within its regularity, presents rhythmically or arrhythmically an irregularity. When an irregular pulse is palpated, a sinus arrhythmia should be suspected, and if the irregularity is total it may be atrial fibrillation or atrial flutter with variable block.
The regular-irregular pulse can be due to premature atrial or nodal (supraventricular) contractions or premature ventricular contractions.
Among the regular and rapid heart rhythms are sinus tachycardia, 'which has already been described, supraventricular tachycardias, atrial flutter with a normal ventricular response, and ventricular tachycardia. Supraventricular tachycardia (160-200 beats / min) is a rapid rhythm that occurs in paroxysmal episodes and affects young individuals without evidence of heart disease; In these cases, the response to vagal stimulation may be acceleration, slowing down, and there may also be no changes. Atrial flutter 150-160 beats / min) with normal ventricular response is a rapid rhythm, and there is usually a partial block in the atrioventricular node. The atrial rhythm is around 300 beats per minute, and the response to vagal stimulation is the same as that of the previous arrhythmia. When there is a higher degree of AV block, for example 4 to 1, and this block is maintained continuously, the pulse rate will be 60-100 beats / min, with a vagal response identical to the previous one.
Ventricular tachycardia is an arrhythmia with a very poor prognosis and precedes ventricular fibrillation and sudden death. It is usually associated with severe heart disease, originates in the ventricles and has a rate of 150-200 beats / min; furthermore, it does not respond to vagal stimulation.
Among the regular and slow heart rhythms, sinus bradycardia, already described in a previous paragraph, second-degree AV block, and complete AV block should be mentioned.
In second-degree AV block (35-60 beats / min), atrial impulses fail to reach the ventricles, and only some can depolarize the ventricles on a regular basis; the most frequent cause is the use of digitalis. In complete AV block, there is a total or complete block of the normal atrioventricular conduction pathways. Ventricular beats originate from the ventricles themselves. The most common cause is myocardial infarction.
Atrial fibrillation, variable response atrial flutter, and sinus arrhythmia constitute irregular rhythms. In atrial fibrillation, P waves cannot be seen on the electrocardiogram (ECG). The heart rate is directly related to the degree of existing blockage. In sinus arrhythmia, the rhythm variation is cyclical; it increases with inspiration and decreases with expiration.
Among the regular-irregular rhythms are extrasystoles or premature contractions of supraventricular origin, whether atrial or nodal, and ventricular extrasystoles.
Alterations in amplitude and shape , a) Decrease in the amplitude of the pulse wave. A lower amplitude of the pulsatile wave indicates a decrease in the ejection volume, either due to an obstruction behind the ventricular pump (mitral stenosis) or in front of it (aortic stenosis). In mitral stenosis, the pulse wave, although quantitatively decreased, will retain its normal shape. In aortic stenosis, because the obstruction is ahead of the ventricular pump, the pulse wave must be prolonged in time, thus fighting against the obstruction and altering its shape.
Parvus pulse (Figure 16-1, A). It is a small and loose pulse, of low amplitude and characteristic of all states of low minute volume, where the systolic and diastolic pressure figures are close to the mean arterial pressure. It is a small, but normal pulse and can be found in low-grade aortic, mitral, severe pulmonary and tricuspid stenosis, in significant pulmonary hypertension, in myocardial infarction and in any situation associated with a low minute volume (shock, constrictive pericarditis).
Filiform or decapitated pulse . It is the characteristic pulse of shock, whatever its cause; it is characterized by being very small and because the cusp is not palpable.
Anacrotic pulse . It is a sustained pulse, as in plateau, of slow ascent and in which the cusp is delayed of the pulse wave. It is the characteristic pulse of moderate and severe aortic stenosis. In the ascending wave (anachrotic), a notch (anachrotic notch) can be palpated, which will be the earlier the greater the stenosis. This slow rise in the pulse wave disappears when the heart rate increases.
Bisferiens or double-beat pulse (Figure 16-1, B). This pulse is characterized by the presence of two twin waves separated by a central wave. The two waves are similar and a deep anacrotic notch separates them. It is a characteristic pulse of double aortic injury, insufficiency and stenosis, with a predominance of the former. It can be considered as a variant of the anacrotic pulse, in which the notch is very delayed due to the existence of a mild aortic stenosis, and is deep due to the large systolic volume due to aortic regurgitation.
b) Increase in the amplitude of the pulse wave . It indicates an increased left ventricular ejection volume, and consequently a wide differential pressure (Figure 16-1, C). The alteration of its shape will depend on the existence of abnormalities in the outflow tract.
Celer or water hammer pulse . It is characteristic of aortic regurgitation and patent ductus arteriosus. It is a pulse of increased amplitude and in a striking way: sudden ascent, with a tiny cusp, and rapid descent, which causes a jumping pulse.
In aortic regurgitation, blood regurgitation produces increased ventricular diastolic filling and increases the initial tension of myocardial fibers.
These patients have a higher peak pressure with a short ejection phase and systolic pressure drops abruptly, leading to the appearance of a large, abruptly onset pulse wave with rapid collapse.
Bouncing pulse . It is also characterized by a large percussive wave, but with a rounded shape. It is found in hyperkinetic states: hyperthyroidism, heat, Paget's disease, alcoholism, gravid uterus, beriberi. In reality, there is only one difference in intensity between the celiac pulse and the jumping pulse. In both the stroke volume is increased, but in the celler the low aortic resistance produces a rapid fall in the pulse wave.
Other pulses are also described:
Dicrotic pulse . It is a double pulse without any clinical significance. The pulse wave is continued with the dicrotic wave, which occurs in diastole, constituting a double pulse. It can be found in young patients affected by an infectious disease such as typhoid fever or endocarditis.
Paradoxical pulse (Figure 16-1, D). In the normal subject, the pulse quickens during inspiration and slows down on expiration, with no changes in its volume. If the pressure is recorded in the pulmonary vascular tree and in the systemic vessels, an increase in pulmonary resistance will be detected during inspiration, with a slight drop in systemic tension. The paradoxical pulse is an exaggeration of the events that normally occur: it is characterized by disappearing or becoming very small during inspiration. We find this pulse in constrictive pericarditis, in tension pericardial effusions and in some low minute volume cardiomyopathies. When it is found unilaterally, it is in the presence of a scalene syndrome.
Alternating or alternating pulse (Figure 16-1, E). It is characterized by being a rhythmic pulse, but with uneven beats, in which large and small waves alternate. We can find it in left ventricular failure, aortic stenosis, severe systemic arterial hypertension, myocardial infarction and atrial flutter. Together with auscultation of the third sound, the alternating pulse is a finding of semiological value in left ventricular failure.
Bigeminate pulse (Figure 16-1, F). It is characterized by presenting the pulse waves grouped in pairs. It is usually caused by a normal contraction, followed by another premature contraction (extrasystole) and smaller. These waves are separated from subsequent waves by a compensating pause. 3: 2 atrial blocks also present with a bigeminate rhythm, but unlike the previous case, both beats are equal in shape and time, and are separated from the subsequent group by a space twice that of the normal cycle.
Trigeminated pulse . It is characterized by presenting the beats grouped in waves of three. We find it in 4: 3 atrioventricular blocks and in double extrasystoles that are coupled to the normal beat.
Alterations in tension . The increased tension of the pulse wave should make one suspect the possibility of arterial hypertension.
BREATHING DISORDERS
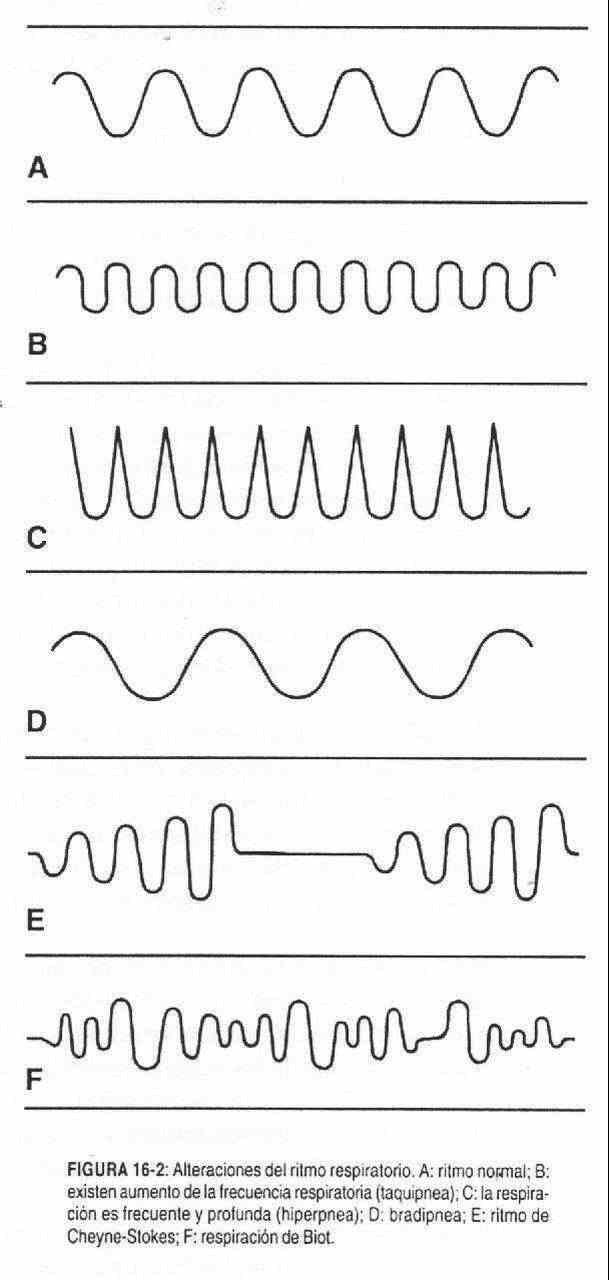 As a consequence of the volume and pressure changes produced by the respiratory muscles, air flows into the thorax. Expiration occurs due to the relaxation of these muscles and the elasticity of the thorax, which allow the air that has entered the lungs to escape.
As a consequence of the volume and pressure changes produced by the respiratory muscles, air flows into the thorax. Expiration occurs due to the relaxation of these muscles and the elasticity of the thorax, which allow the air that has entered the lungs to escape.
Among the alterations that can occur in the respiratory act, the following should be mentioned:
1. Alterations in respiratory rate and rhythm . Tachypnea (Figure 16-2, B) is an increase in respiratory rate that is accompanied by an increase in minute volume. On the other hand, if breathing is shallow, tachypnea may be due to pleural pain, fever, elevation of the diaphragms.
Bradypnea (Figure 16-2, D) is a decrease in respiratory rate; it is seen in collapses and comas, usually with increased intracranial pressure.
Kussmaul Breath . It is characteristic of states of metabolic acidosis (diabetic acidosis, renal acidosis, or due to drugs). It is characterized by being a respiration that has increased in depth (Figure 16-2, C) in an attempt to wash away the accumulated carbon dioxide, and that can have a normal, slow, or fast rate.
Cheyne-Stokes respiration . It is an irregular breathing rhythm that is interrupted for about 15 seconds and begins with small respiratory movements that then become faster and deeper until they stop again (Figure 16-2, E). This entire cycle can last one minute and comprise, in that period, about thirty inspiratory movements. This respiratory rhythm is found in those patients in whom the sensitivity of the respiratory center to carbon dioxide is diminished.
Biot breath . It is another irregular respiratory rhythm, which, unlike the previous one, does not show any periodicity. Slow respiratory movements are observed, alternating with rapid movements, which at other times present as superficial respiratory movements and at others as deep (Figure 16-2, F). Its most important characteristic is that it lacks rhythm.
2. Alteration of the inspiration / expiration ratio . When there is an obstruction to airflow (asthma, emphysema, chronic bronchitis), the body must increase the chest pressure to breathe out the air, which is reflected in a prolonged expiration and in the use of the expiratory muscles with fixation of the abdominal muscles . Expiration is prolonged above inspiration, breaking the normal inspiration / expiration ratio of 3: 1.
3. Hyperventilation . It is the increase in respiratory movements, which leads to a decrease in the partial pressure of carbon dioxide. It occurs in acidosis or when nerve centers are irritated by bacterial action or by chemical agents.
4. Apnea . It is the arrest, of greater or lesser duration, of breathing. It can be seen in brain tumors, meningitis, intracranial hypertension, and thrombosis of the vertebral arteries.
ABNORMAL FINDINGS IN BLOOD PRESSURE
Among the abnormal findings that can be obtained when taking blood pressure are (see table below):
1. High blood pressure . It is the increase in blood pressure, systolic or diastolic. It can be of unknown or essential cause or secondary to other conditions. The finding of elevated blood pressure, in a single measurement, does not define the patient as hypertensive. Therefore, it should be controlled at some other time during the physical examination, since modifications occur with anxiety states. Blood pressure is a dynamic and not a static parameter. To define arterial hypertension, high blood pressure figures in both arms must be found in two or three medical visits.
Elevation of systolic pressure can occur in patients with increased cardiac output.
In these patients, the differential pressure increases due to an increase in the output volume. It is the picture produced by anemia, hyperthyroidism, beriberi, alcoholism. With age, the elasticity of the arteries decreases, producing an increase in systolic blood pressure, known as systolic hypertension. Arteriovenous fistulas, pregnancy, and aortic regurgitation lower diastolic pressure. The pressure may be increased in one limb only or in the upper limbs and not in the lower limbs as in coarctation of the aorta.
2. Orthostatic changes in blood pressure . Orthostatic changes in blood pressure are due to dysfunction of the autonomic nervous system, as occurs in diabetes or treatment with hypotensive drugs, or when there are volume losses such as bleeding or dehydration. The 10 mm Hg drop with the change in position of the patient, from lying down to sitting (tilt test), indicates a lack of volume, caused by loss of blood or fluids. In turn, if with the upright position there is no decrease in blood pressure, but there is an increase of 25-30 beats per minute in heart rate, this finding may be a sign of effective hypovolemia.
3. Hypotension . It can be present in the pictures of shock, adrenal insufficiency and cachexia. In an asymptomatic patient, the finding of a maximum pressure of 90 mm Hg is within normal limits. One cannot speak of shock without a clear repercussion of low blood flow at the level of the fundamental organs: oliguria, tachycardia, excitement, clouding.
4. Arrhythmias . When the patient is a carrier of a cardiac arrhythmia (example: atrial fibrillation), blood pressure must be recorded several times in order to later obtain an average of the values; these patients show changes in flow and resistance, and auscultation can vary from beat to beat. In such cases the lowering of the pressure cuff should be done slowly.
5 Auscultatory well . It is a period of silence between the maximum and minimum pressure that can be found in some hypertensive patients. In these, palpation should be used before auscultating the pressure, to detect the first palpated beat, which will mark the systolic pressure.
6. Difference greater than 10 mm Hg . Normally the difference in blood pressure measured in both arms should not be more than 10 mm Hg. A greater difference is seen in cervical rib syndrome, arterial occlusion, dissection of the aorta, external occlusion of the artery (due to tumor compression), coarctation of the aorta, Takayasu arteritis, and also when there is an noticeable difference in the size of both arms, or after the Blalock-Taussig operation (sympathectomy), or by error in measurement.
7. Paradoxical or alternating pulse . It is the drop of 10 or more mm Hg that occurs during inspiration in patients with pericarditis, asthma or emphysema.
ABNORMAL FINDINGS IN HEIGHT AND WEIGHT
Weight control is used to determine nutritional status and water metabolism disorders. Weight changes that occur within hours or a few days are generally associated with disorders of water metabolism, and are of utmost importance in the follow-up of ascites or edematous patients. Weight is very important to control the development of children and pregnant women and it is also used for the dosage of certain medications. The patient should always be measured and weighed, to later determine if it is within normal values for their age, race and physical build, and thus be able to define if there is a lack or excess weight. It should also be compared to your usual weight.
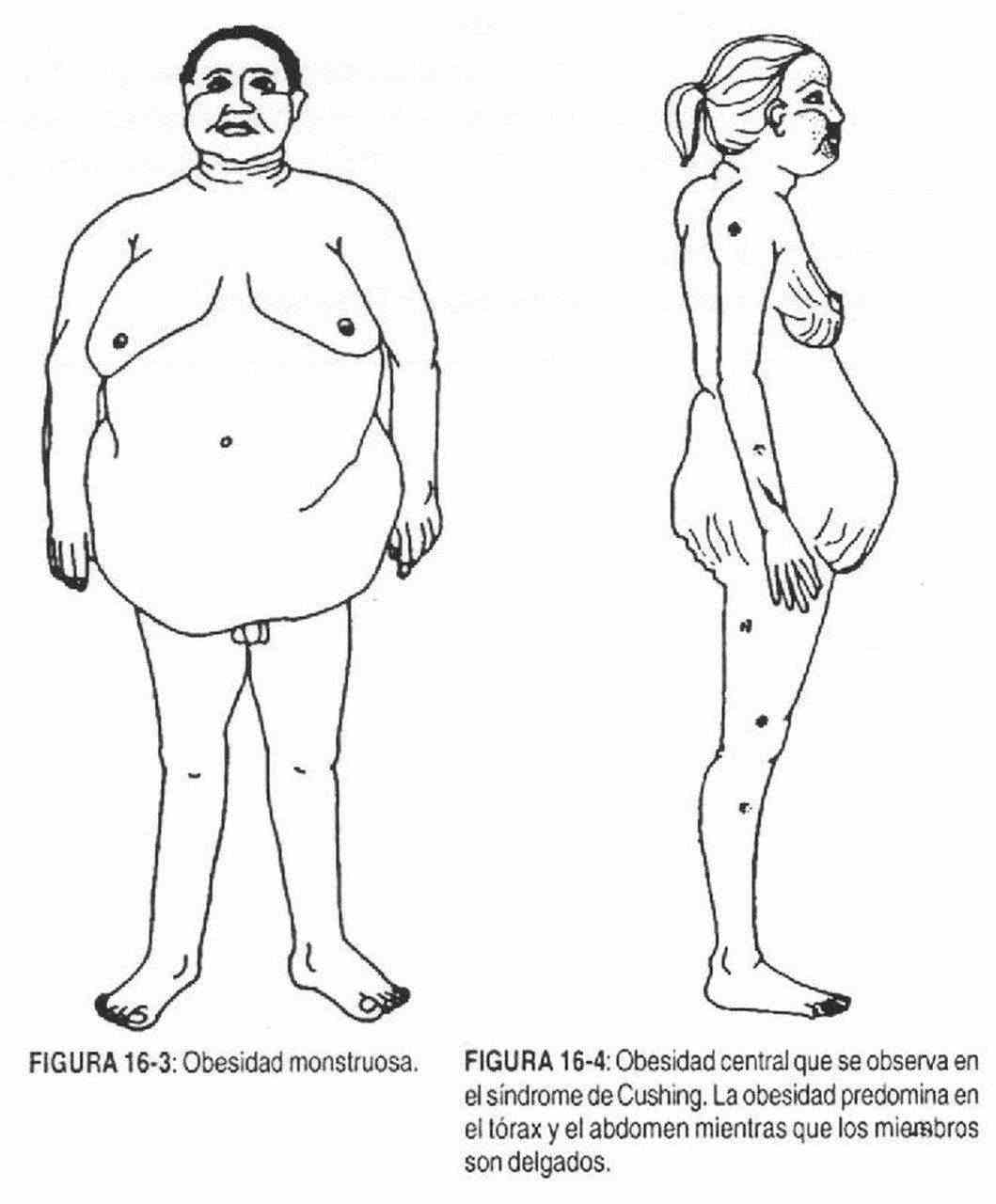
Obesity . It is the arbitrary optimal weight increase above 15-20% of that obtained in a population study for that age, height and sex, with correction for bone structure. Adiposity, on the other hand, occurs in those with normal weight, but with an excessive amount of fatty tissue.
Some types of obesity have been described, such as gynecoid (accumulation of fat in the lower half of the body), android (in the upper half), and monstrous (reaches gigantic proportions) (Figure 16-3). Obesity can also be centripetal or central as in Cushing syndrome (Figure 16-4) and centrifugal as in common obesity.
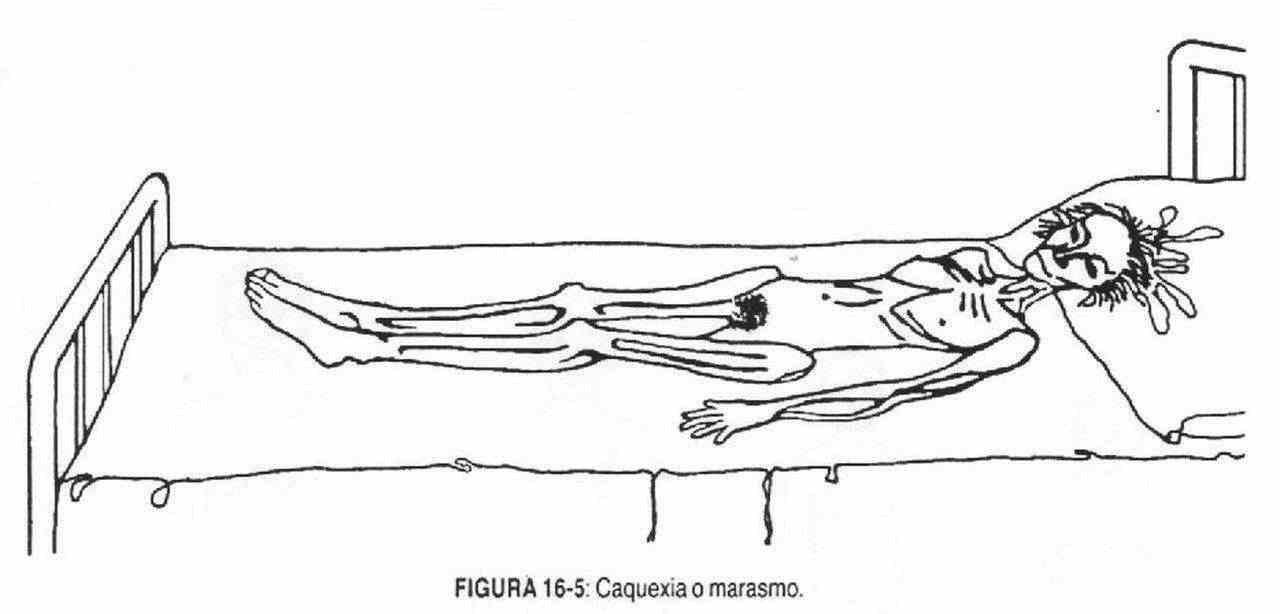
 Slimness . It is the opposite state to the previous one, and it is characterized by the lack of fatty tissue. Cachexia or marasmus (Figure 16-5) is the extreme state of thinness or starvation, with loss of muscle mass and fat, sunken eyes, and prominent cheekbones.
Slimness . It is the opposite state to the previous one, and it is characterized by the lack of fatty tissue. Cachexia or marasmus (Figure 16-5) is the extreme state of thinness or starvation, with loss of muscle mass and fat, sunken eyes, and prominent cheekbones.
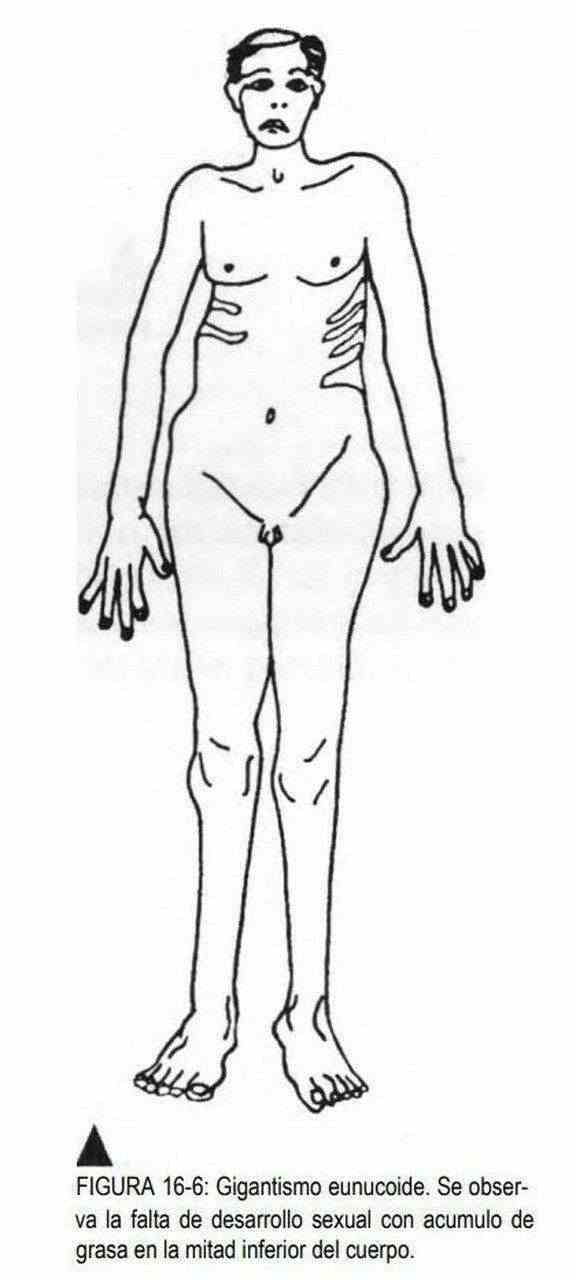
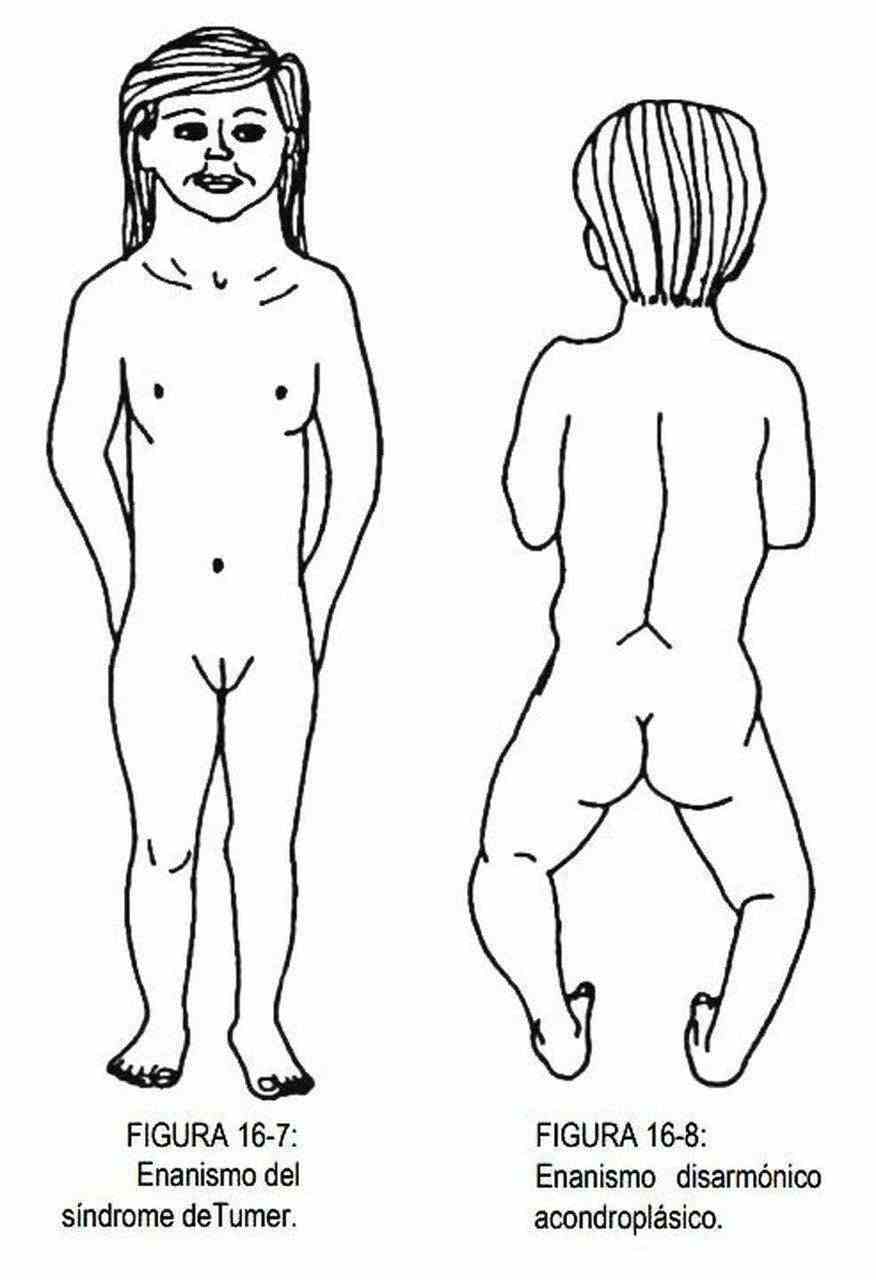
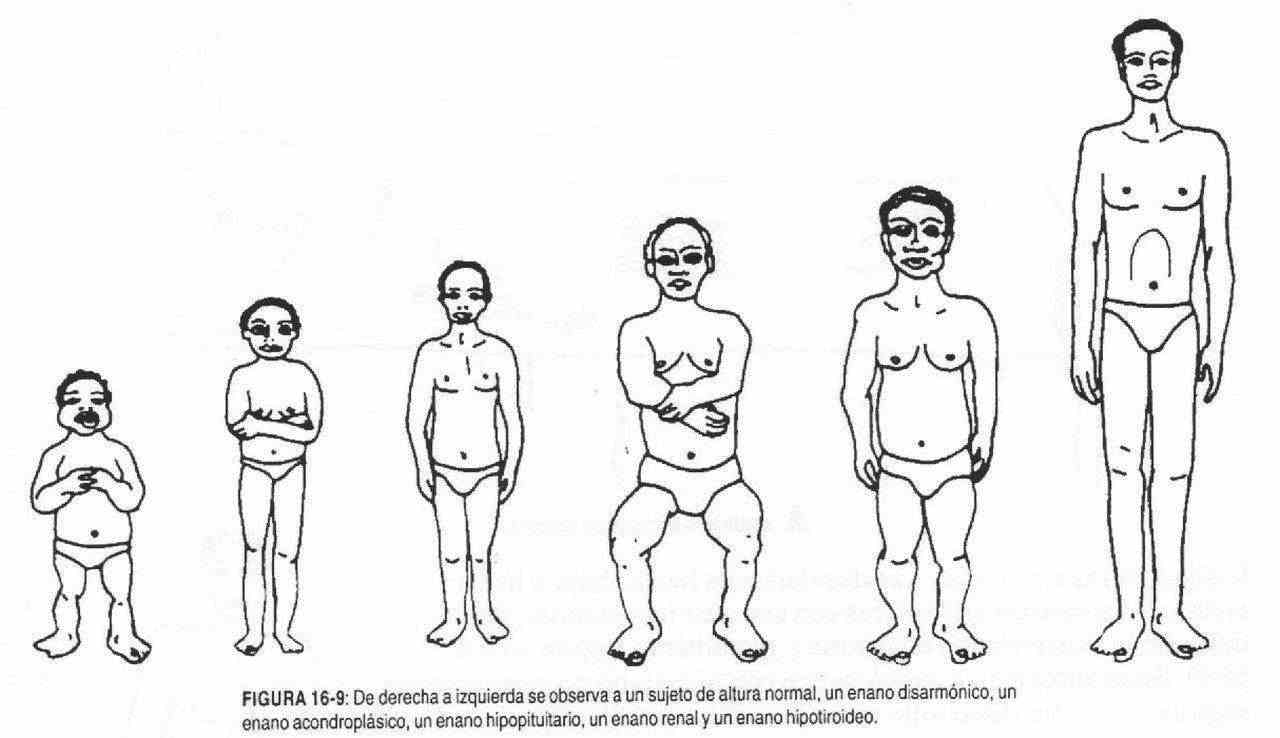
 Height is also tabulated according to age, race, and sex. The downward or upward deviations of the arithmetic means with their standard deviations will determine the existence of dwarfism and gigantism (Figures 16-6 to 16-9). These alterations can be harmonic or disharmonic, depending on whether or not there is a relationship with the size of the limbs, and with or without sexual development.
Height is also tabulated according to age, race, and sex. The downward or upward deviations of the arithmetic means with their standard deviations will determine the existence of dwarfism and gigantism (Figures 16-6 to 16-9). These alterations can be harmonic or disharmonic, depending on whether or not there is a relationship with the size of the limbs, and with or without sexual development.
ABNORMAL FINDINGS IN TEMPERATURE
A patient is said to be feverish when his axillary temperature is above 37 ° C, or orally above 37.3 ° C, or rectally above 37.5 ° C. When the decrease in temperature occurs in a member, it is due to a decrease in blood supply. Peritoneal inflammation produces an axillo-rectal difference greater than one degree centigrade.