Luis Leone
The following chapter aims to introduce students to the beginning of the basic study of the knowledge of cardiac arrhythmias, denoting that the study in greater depth of the intimate mechanisms and types of arrhythmias is reserved for the in-depth advance of specialists. Permanent advance in electrophysiological and pathophysiological knowledge of heart rhythm disorders is constantly updated, as well as study and treatment methods.
We define cardiac arrhythmias as those disorders that alter the normal sinus rhythm of the heart, both in the formation and in the conduction of the impulse.
Excitable cardiac cells have essential properties such as automatism and conduction, these characteristics allow the cells of the cardioconnector system to differentiate from the myocardial fibers responsible for contraction.
When we began to study electrocardiography, we pointed out that the difference between automatic and contractile cells seems to reside in the different behavior in phase IV, which shows spontaneous depolarization in the former, which allows them to reach the threshold potential.
When the formation of the sinus stimulus is depressed or canceled, there are secondary pacemakers such as those of the atrioventricular junction, bundle of Hiss or its branches and Purkinje fibers that can passively or save the command of the heart to keep it beating. The rhythms that are produced will do so with a lower frequency when the ectopic focus is more peripherally located, this beat is called "escape".
Although automatism by definition is spontaneous, it can be modified to a greater or lesser degree by the neurovegetative system, through cholinergic or vagal discharges that slow it down, or sympathetic discharges that on the contrary accelerate it.
The mechanisms involved in cardiac rhythm disturbances are grouped into two main categories 1) by abnormal or increased impulse formation 2) by reentry.
Reentry is installed when an impulse does not extinguish after having propagated through the heart, but persists and re-excites it after the end of the refractory period. The mechanisms that participate in the abnormal formation of the cardiac impulse include increased automatism, which is observed in the presence of conditions that reduce transmembrane potential, such as ischemia, necrosis, or situations that alter ionic channels, determining an increase in intracellular calcium. They can also develop due to the effects of medications, antiarrhythmics or congenital alterations that determine early post-depolarizations. These are transmembrane potential oscillations that appear after the repolarization process has been completed, and when they reach the threshold potential they cause triggered responses.
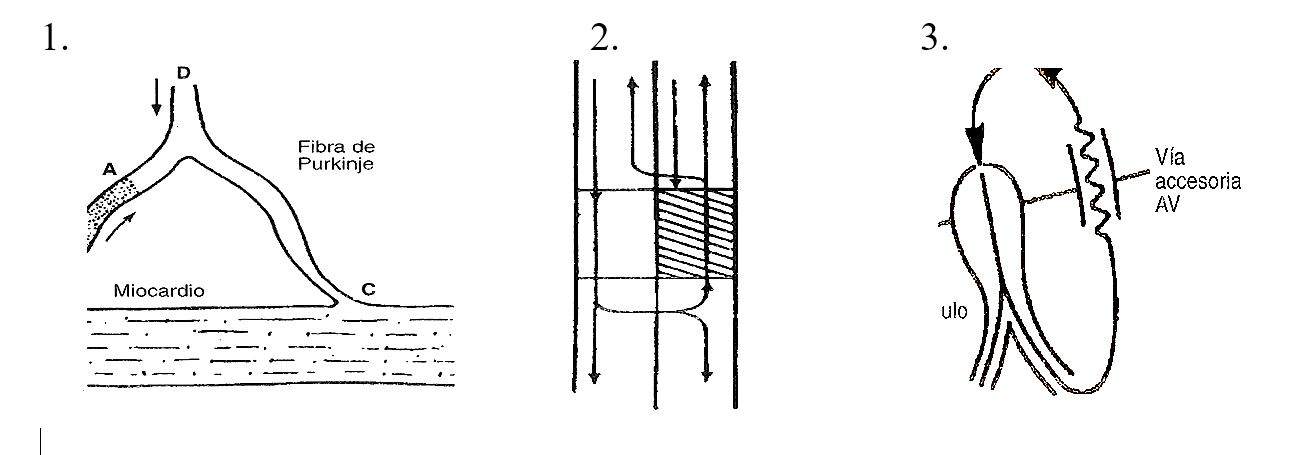
Fig. 1 Mechanism of reentry in a purkinje fiber, the segment denoted as A presents directional block and depressed conduction. The stimulus that descends through D is blocked in A, continues its conduction through C and then re-enters through A in a retrograde manner. 2) In a linear representation the stimulus is blocked in the shaded area in a descending way, continues on the right and once recovered it can be conducted in a retrograde way. 3) Mechanism of re-entry in the case of participation of an accessory pathway.
The autonomic nervous system is the one that modulates normal and abnormal electrophysiological mechanisms, clinically we can observe the balance between sympathetic and vagus through heart rate. For this reason, their interrelation in the participation of cardiac arrhythmias is very direct.
In the generation of an arrhythmia, the following intervene:
a) substrate: determined by any heart disease, denoting that heart failure and hypertrophy are arrhythmogenic "per se."
b) clinical arrhythmia: whatever it may be.
c) Autonomic nervous system: determining vagosympathetic relationship in its arrhythmogenic role, as in the case of post-effort tachyarrhythmias.
Both adrenergic and vagal stimulation can trigger atrial fibrillation, due to alterations in refractoriness, and conduction.
The arrhythmias that are observed in mitral prolapse have a predominantly adrenergic sympathetic profile
Examples of mechanisms of atrial and ventricular arrhythmias.
| Tachyarrhythmia | Mechanism | Heart rate |
| Sinus tachycardia | Automatism | > 100 |
| Atrial flutter | Reentry | 150-350 |
| Atrial fibrillation | Reentry | 250-450 |
| Tps for intranodal reentry | Reentry | 120-250 |
| Tps by accessory route | Reentry | 150-250 |
| Ventricular tachycardia | Re-entry. Automatism (rare) | 140-300 |
| Vd outflow tract tachycardia | Triggered activity | 120-200 |
| Torsade de pointes | Triggered activity | 200 |
Both adrenergic and vagal stimulation can trigger atrial fibrillation, due to alterations in refractoriness, and conduction.
The arrhythmias that are observed in mitral prolapse have a predominantly adrenergic sympathetic profile
The slight changes in heart rhythm that occur with respiratory movements and neurovegetative influences are called sinus arrhythmias.
For an ectopic stimulus to take control of the heart, it needs to meet the following conditions:
It must be of supraliminal intensity.
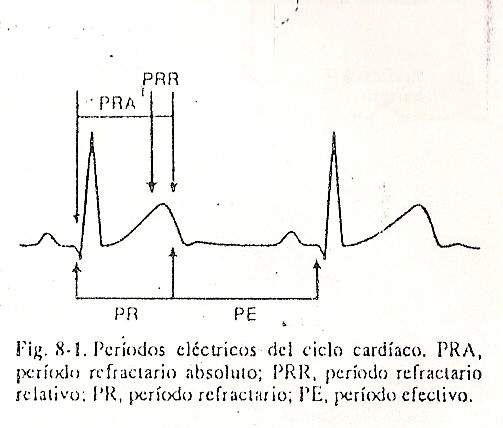
It must occur in the atrial or ventricular excitable period, depending on the case; that is, the refractory period must not fall. The ventricular refractory period corresponds to the time that elapses from the beginning of ventricular activation, that is, the beginning of the QRS, until near the end of ventricular repolarization, between the vertex and the end of the T. To the first part of the period Total refractory period is called the absolute refractory period, and in it no stimulus, even with intensity much higher than the threshold, is capable of producing a propagated response. The last part of the refractory period is called the relative refractory period; It is of shorter duration, and in it a stimulus, to spread, needs to have a greater intensity than is required during the excitable phase.
The phase of the cardiac cycle between the end of the refractory period and the beginning of the ventricular QRS complex; this phase corresponds to ventricular electrical diastole, and in it ventricular excitability remains constant, that is, the intensity of the stimulus required to produce a propagated response is almost the same throughout its duration (Fig. 8-1).
The tissue surrounding the focus of abnormal automatism must have sufficient capacity to conduct the stimulus. For example, if conduction is very slow in these areas, the next sinus stimulus will have enough time to descend into the ventricles and depolarize them before the ectopic stimulus
If the ectopic stimulus is atrial and arises during the excitable phase of the atrium but finds the nodule in a refractory period, there will be atrial depolarization with AV block for this stimulus. A frequent example of the blockage of the ectopic stimulus is the one that refers to the so-called blocked atrial extrasystoles. The atrial ectopic stimulus spreads through the already recovered (i.e. excitable) atrial muscle but reaches the junctional tissue in a refractory period, thereby blocking the AV node or His bundle and does not descend to the ventricles .
It is useful to remember which are the semiological characteristics that allow to diagnose with certainty if a certain trace is commanded by a sinus or physiological rhythm.
They are:
sequence of P, QRS and T waves that occur regularly;
P wave with a projection around + 60º in the frontal plane, justifying its negativity in aVR and isodifasism in aVL;
PR interval between 0.12 and 0.20 seconds, and heart rate between 60 and 100 beats per minute.
Bradyarrhythmias and atrioventricular conduction disorders
Sinus bradycardia. Sinus rhythm whose rate is less than 60 beats per minute is described as such.
The trace has all the characteristics of a correctly originated and propagated stimulus, albeit slow, with an interval between the P waves of less than one second.
It can simply be an expression of an exaggerated vagal tone, as observed during night rest in athletes and in general in individuals with a predominance of the parasympathetic system; On occasions, in a pathological form it can appear in hyperthyroid patients, in patients with intracranial hypertension, in jaundice, in malnourished patients and in some infections such as typhoid fever.
Sinoatrial block. In these cases, the sinus node does not issue orders and in others there is a delay or blockage in the conduction of the stimulus from the sinus node to the surrounding atrial tissue. Consequently, the atria and ventricles are not paced and the tracing shows a prolonged pause. Three variants are recognized in this type of block (Fig. 8-2):
First degree sinoatrial block, which cannot be documented by surface ECG.
Second-degree sinoatrial block, of the Wenckebach type, where the PP intervals become progressively longer until a prolonged pause appears between two successive beats (a physiological sinus arrhythmia or associated with respiratory movements should be ruled out), or of the Mobitz type, where the great pause turns out to be a multiple of the interval between two successive normal P waves.
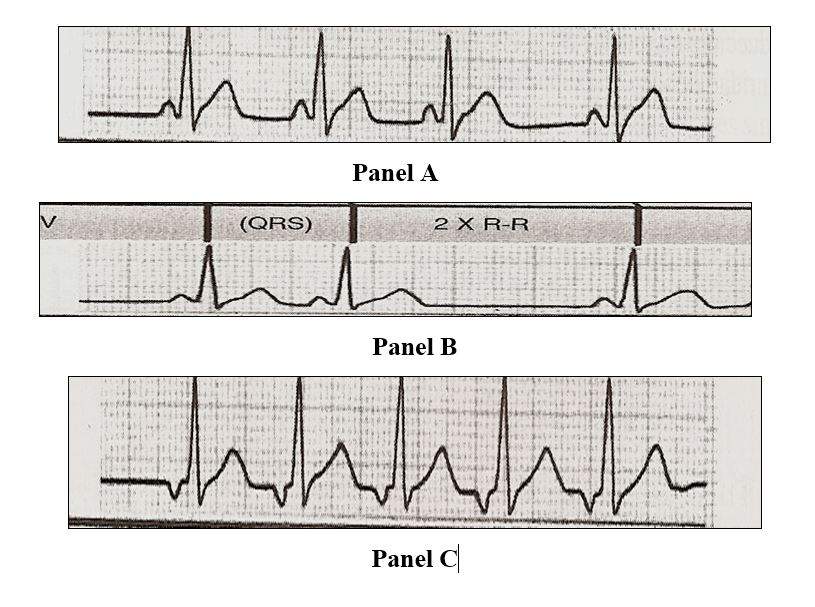
Fig 8-2 Sinoatrial blocks. Panel A of Grade 2 with Wenckebach periods. Panel B Blocking SA type Mobitz. Panel C Complete S_A block, no sinus stimulus reaches the ventricle, the rhythm is generated by a low atrial focus (they correspond to lead D2).
Third-degree sinoatrial block, characterized by asystole, that is, lack of registration, due to short or long pauses that are multiples of the PP interval.
Any of these blocks can occur in healthy people with exaggerated vagal tone, except in cases of third degree sinoatrial block, which are always pathological. It should not be forgotten that certain drugs such as digitalis, acetylcholine, quinidine, and potassium salts can be the cause of its appearance. At other times they are an expression of coronary disease.
Sinus arrest. It is the cessation of sinus stimulus production, and is characterized by the absence of P waves, absence of the QRS and the T wave, pauses that are not multiples of two sinus PP intervals. It is difficult to differentiate it from sinoatrial blocks, although in the latter there are usually P waves of variable morphology as a consequence of atrial fusion beats and nodal or atrial leaks. It can be found in apparently healthy patients who show exaggerated vagal tone, in cases of intoxication with drugs such as digitalis and quinidine, in cardiomyopathies and in coronary heart disease.
Rhythm of union. Idioventricular rhythm is a manifestation that appears when there is a depression of the sinus node and the other subsidiary pacemakers or a high-grade AV block. The presence of "narrow" QRS shows its origin in the bundle of His or in its branches and "broad" when they originate in the lower sectors.
Autrioventricular block. It happens when the conduction of the stimulus from the atria or ventricles is delayed or totally interrupted, a situation that can be transitory, intermittent or permanent.
Classically, first-degree, second-degree, and third-degree or complete blocks are identified, which will be reviewed successively (Fig. 8-3).
First degree atrioventricular block. It is a delay at the level of the AV node that exceeds the maximum physiological limits, since the ECG recognizes the prolongation of the PR interval above 0.20 sec. The most common causes are: coronary heart disease, rheumatic fever, congenital conditions (eg, atrial septal defect), etc.
Second degree atrioventricular block. Two variants are described, type 1 or Wenckebach, and type 2 or Mobitz. Type 1 is the most common form, and in this case each atrial stimulus finds it increasingly difficult to cross the AV node; this translates on the ECG into a proportional prolongation of the PR interval until a P wave is not conducted because it cannot penetrate the atrioventricular junction. Therefore, such a sinus wave will not be followed by a ventricular complex; When the next stimulus reaches the AV node, it will have recovered and the PR will be normal. The subsequent heartbeat will again show a prolonged PR, until finally the blockage recurs. It is also an expression of conditions such as coronary heart disease or the action of drugs that decrease conduction at the AV node level.
Type 2 or Mobitz is less common. In this type of block, the AV junction intermittently collapses in conduction of the atrial stimulus, the PQ or PR are constant but suddenly the sinus order is not transmitted to the ventricles and the P wave is not followed by a QRS. The ventricular complex can be wide or normal, and this depends on whether or not there is an associated bundle branch block. The causes of this disorder are the same as those that produce second-degree Wenckebac-type AV block
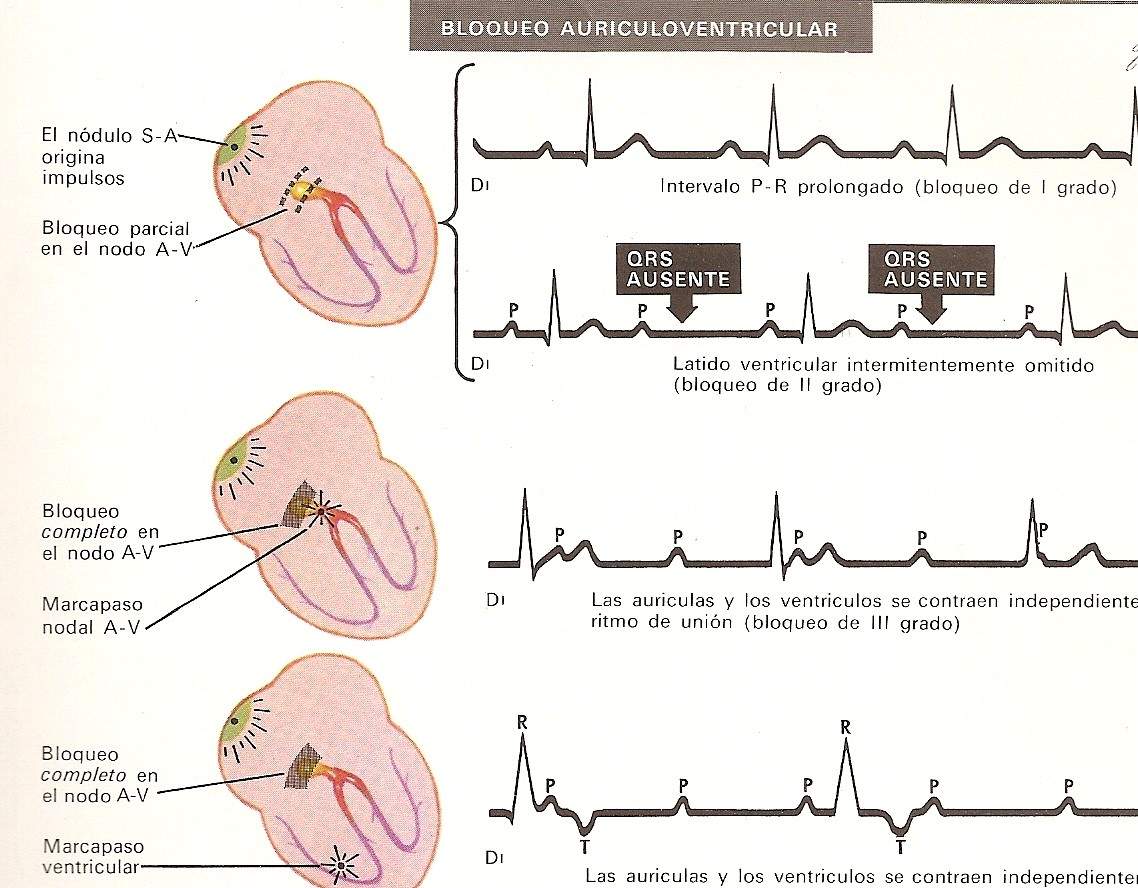
Complete or third degree atrioventricular block. In all these cases, atrial stimuli are blocked at the AV junction, so life can only be sustained if other impulses originate in a region distal to the Aschoff-Tawara node. When new stimuli emerge in the vicinity of the AV junction, the ventricular discharge or peripheral heart rate will be around 50 beats per minute. Below this figure, the morphology and duration of the QRS will have a normal duration; If, on the other hand, the accessory pacemaker is located at a more distal level, there will be an idioventricular rhythm and in this case the QRS will be wide and aberrant, simulating a bundle branch block. In these circumstances the peripheral rate falls to critical limits of 30 to 35 beats per minute.
Atrioventricular dissociation. We speak of AV dissociation when the atria and ventricles beat independently but the ventricular rate is slightly faster than the atrial rate, giving rise to an inverse situation to that which occurred with blocks.
In this arrhythmia, therefore, there are two natural pacemakers that compete with each other to dominate cardiac activity: the sinus node stimulates the atria, while the junctional tissue does so with the ventricles almost in unison. Thus, when the order of the sinus node arrives at the AV node, it finds it in a refractory period.
This situation differs from complete or third degree AV block because in the latter the sinus stimulus can never be transmitted to the ventricles, while in dissociation this can happen if the node is found in a non-refractory period; furthermore, complete AV block responds to an organic cause, whereas dissociation is usually functional and usually reversible. This arrhythmia is produced, in general, by a marked vagal stimulus or by drugs such as digitalis, quinidine, etc. Other times the cause is an acute condition, a myocardial infarction, high blood pressure, and sometimes its origin is uncertain.
Supraventricular arrhythmias
This term includes sinus tachycardia, atrial extrasystoles, paroxysmal atrial tachycardia, junctional extrasystoles, nodal tachycardia, atrial flutter, and atrial fibrillation.
Sinus tachycardia It is arbitrarily defined as sinus rhythm if the rate is greater than 100 beats per minute, although in young people and during exercise it can reach 180 beats per minute. P waves have a normal electrical axis that guarantees their sinus origin. When the heart rate is very high, the atrial waves are confused with the preceding T waves and both the PR and the QT tend to shorten. Tachycardias of this type occur in normal people during exercise, anxiety or after large intakes of some drinks such as coffee, tea, etc. It can be seen in numerous daily clinical situations such as hyperthyroidism, heart failure, febrile diseases and in the course of acute myocardial infarction, as an expression of anxiety, shock, etc.
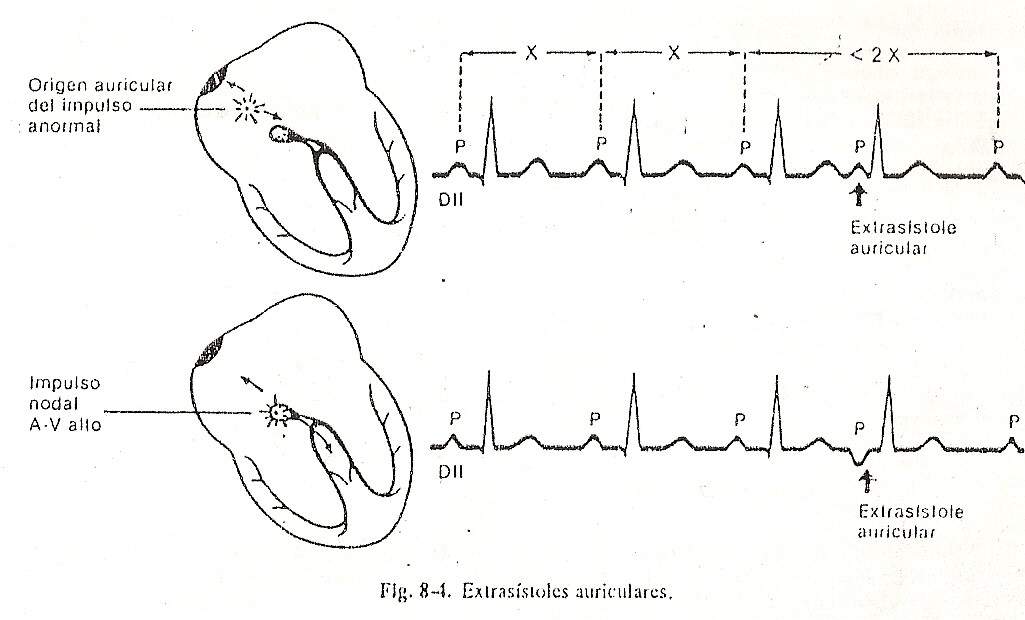
Atrial extrasystoles (Fig. 8-4). They indicate that the atria have been stimulated before the regular sinus beat emerges by the action of an atrial ectopic focus. The electrocardiographic tracing shows:
Premature or anticipated P waves that may be superimposed on the preceding T wave, and therefore followed by a QRS and its normal T wave. Other times the atrial extrasystoles are blocked and fail to stimulate the ventricles.
The PR interval of atrial extrasystoles is generally longer than that of the sinus impulse.
The QRS and T wave that follow extrasystole have the same configuration as that of a sinus rhythm complex, although they can sometimes show aberrant conduction when finding some part of the conduction system in a refractory period. In these cases, the most common is that an image of the right bundle branch block is recorded.
These extrasystoles can be found in normal people or in pathological situations such as heart failure, myocardial infarction, atrial ischemia.
SUPRAVENTRICULAR TACHYCARDIA:
Tachycardia is the succession of 3 or more beats originating from different sites of the atria or the AV junction at a rate greater than or equal to 100 beats per minute. They can be divided into sustained (duration greater than 30 seconds) or non-sustained (duration less than 30 seconds).
According to the morphology of the P wave, they can be divided into monomorphic or polymorphic, the QRS being normal or showing different degrees of intraventricular aberration.
The causes of these arrhythmias are determined in some cases by an automatic origin and in the highest incidence by reentry mechanisms with or without the participation of accessory pathways.
Supraventricular tachycardias without participation of accessory pathways.
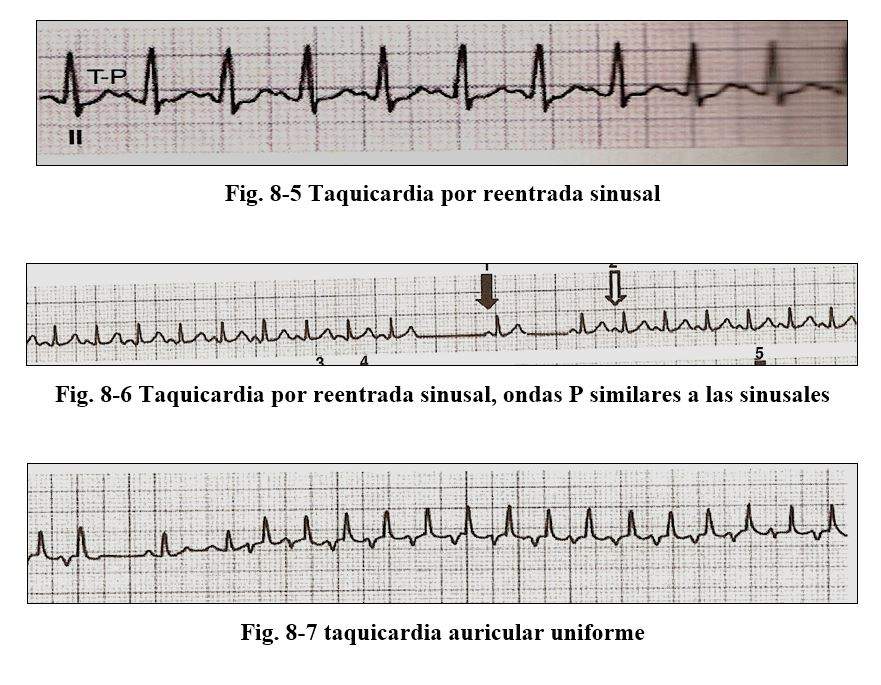
Within this group we find: A) sinus node reentrant tachycardia produces tachycardias of 100 to 160 x 'where the P morphology is identical to sinus with a PR interval similar to baseline. B)
Uniform atrial tachycardia is organized and is characterized by presenting identical P waves and there is an isoelectric line between successive P waves. C) Automatic junctional tachycardias, its frequency is 100 to 130 per minute, the P waves can be retrograde, be earlier during or after QRS, with the condition that when they precede them the PR should not be greater than 0.10 sec. and that when they are after the RP should not be greater than 0.20 sec. D) very rare biderectional tachycardia characterized by an image of right bundle branch block with alternating anterior and posterior hemiblock.
E) chaotic or multiform atrial tachycardia sometimes occurs preceding atrial fibrillation with different P and PR morphologies denoting its origin in different places, it occurs in the elderly and patients with chronic lung disease, with frequencies from 100 to 150.
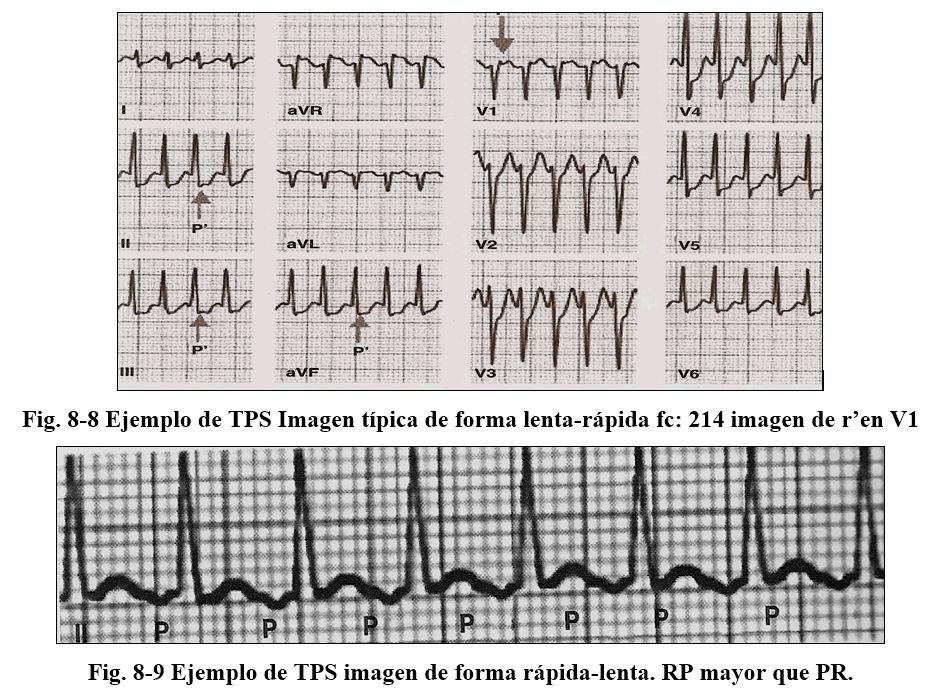
F) Tachycardias due to intranodal reentry, the reentry mechanism occurs because the AV node has 2 conduction pathways (not accessory pathways) with dissimilar electrophysiological properties: one with fast conduction and a prolonged refractory period and another with slower conduction and a longer refractory period. Briefly, these differences that normally do not occur are evidenced by generating favorable conditions to determine this reentry. Its frequency is from 140 to 220 with 1: 1 conduction, presenting the "common" varieties where the impulse descends through the slow path and ascends through the fast path (slow-fast) where the P and QRS waves are registered simultaneously, presenting sometimes in V1 a pseudo r 'wave (Fig. 8-8)
In the fast-slow presentation, the impulse goes down a fast pathway and re-enters the atria through a slow pathway, which is why these are not activated at the same time as the ventricles but later, so the RP intervals are longer than the ventricles. PR intervals.
Paroxysmal tachycardias due to intranodal reentry are frequent, present after adolescence and in individuals who have not presented previous arrhythmic events. These would not be true pathways, but rather large areas of normal atrial connections, in which conduction and refractory properties would vary.
The most frequent causes of these tachycardias are found in healthy patients and on other occasions in hyperthyroidism, pulmonary diseases, and congenital heart disease. They can last for minutes, hours, which is why we call them paroxysmal; up to days causing pictures of tachycardiomyopathy due to its high frequency leading to heart failure.
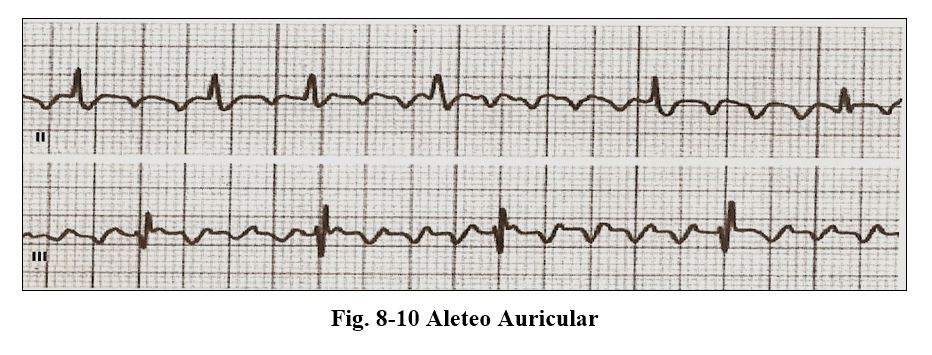
Atrial flutter
It is an arrhythmia with typical electrocardiographic characteristics
The P waves are called F waves, they have a frequency of 240 to 340 beats per minute and between them no isoelectric line is observed, the ventricular response being variable, conditioned by the electrophysiological characteristics of the AV node, presenting a more frequent conduction relationship of type 2: 1 conditioning a ventricular rate of 140 to 170 beats per minute.
Both the flutter and atrial fibrillation occur in the course of countless cardiac, hypertensive, coronary, congenital and pure arrhythmogenic pathologies, having to be diagnosed early due to the high frequencies that they determine and due to the complications that can determine, embolisms, such as re-aggravation of previous pathologies.
Two varieties of flapping are recognized, the “typical” one with anticlockwise caudal head activation with T waves (-) in leads II-III-AVF and positive in V1; the “atypical” presentation with positive and negative II-III-AVF in V1 with hourly caudocephalic activation, its presentation being less than 10%
The mechanism in typical atrial flutter would be a reentry dependent on the cavo tricuspid isthmus (tricuspid ring, inferior vena cava, orifice of the coronary sinus); and not in the case of atypical flapping, which is considered to be due to macroreentrant mechanisms, scars or functional alterations.
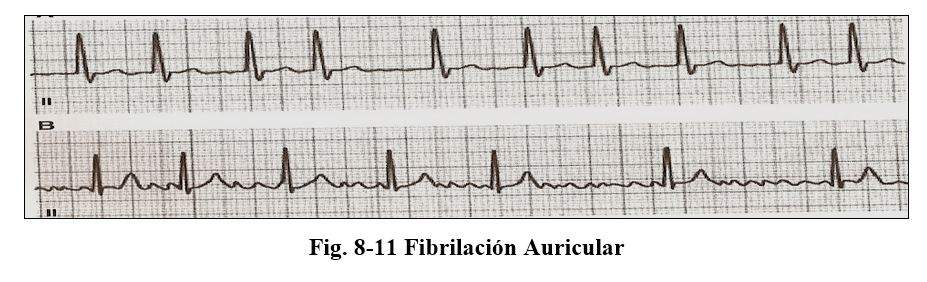
Atrial fibrillation
Atrial fibrillation is the most frequent arrhythmia in adults, its frequency is double that of any other arrhythmia and its incidence increases with age.
The diagnosis of this arrhythmia by ecg is based on: A) absence of waves
P that are replaced by f waves, irregular and variable voltage
B) irregular RR intervals C) variable ventricular response.
Due to their presentation, they are classified as 1.paroxistic 2. Persistent 3.permanent.
The paroxysmal form is the one that reverts to sinus rhythm spontaneously.
The persistent form is the one that requires an intervention that can be pharmacological or cardioversion, depending on the patient's condition.
On presentation, permanent is that which persists despite attempts to return to sinus rhythm.
It is estimated that approximately 6% of those over 65 years of age suffer or have suffered from some form of atrial fibrillation.
The presentation of this arrhythmia in itself does not constitute a cause of mortality, but the risks associated with it increase the total mortality rates and from cardiovascular causes, by favoring the formation of thrombi with the consequent possibility of embolization, systemic, or pulmonary. or both.
It can be admitted that the atria would be in a state of permanent diastole and its electrical frequency would be 400 to 600 beats per minute, a frequency that is blocked at the level of the AV node allowing, according to its refractory period, the passage of some beats and others not conditioning an irregular rhythm with a variable frequency, determining by definition "the most irregular rhythm within arrhythmias"
Among the predisposing factors for atrial fibrillation are:
Heart failure, arterial hypertension, valvular heart disease, myocardial disease, which would be determined by increased pressure in the left atrium.
Due to coronary artery disease, heart attack, chronic coronary heart disease.
Inflammatory: pericarditis, myocarditis, amyloidosis, cardiac surgery
Metabolic disorders: hyperthyroidism.
Presence of atrioventricular accessory pathways.
The mechanism of production of this arrhythmia would be located in the area of insertion of the pulmonary veins in the left atrium, probably determined by the arrangement of myocardial extensions that are oriented from the left atrium to within the pulmonary veins, determining areas of slow conduction that would favor reentry circuits, plus a possible increase in automaticity.
The treatment of this arrhythmia is determined by the presence or absence of hemodynamic decompensation, heart failure, angina pectoris or high ventricular response associated with ventricular precitation, in these cases having to perform electrical cardioversion.
If there are no signs of hemodynamic decompensation and if its presentation is not greater than 48 hours, a pharmacological reversal will be performed. If its presentation is greater than 48 hours or of uncertain time, the procedure is anticoagulation with control of the ventricular rate by means of drugs.
There are currently highly trained centers with appropriate technology to ablate the areas located in the pulmonary veins and definitively prevent recurrences of AF episodes, or AV node ablations with implantation of definitive ventricular pacing.
Sinus Nodule Syndrome
Sinus node involvement can be seen in multiple pathologies such as: myochagasic heart disease, coronary heart disease, hypertensive heart disease, cardiomyopathy, structural abnormalities, neurovegetative alterations, etc.
the alteration is manifested in the ecg by:
Persistent or intermittent severe sinus bradycardia
Sinus arrest periods, interrupted or not by union rhythms, or idioventricular.
AF episodes with delay in sinus rhythm, after reversal.
Episodes of sinoatrial block or tachyarrhythmias alternating with sinus arrest.
These events may or may not be associated with symptoms according to the degree of involvement of the node and the frequency of the arrhythmia, the most frequent presentation is given by episodes of AF alternating with sinus rhythm of low frequency post spontaneous or medical reversion determining lower heart rates 40 beats.
Therapeutic behavior in symptomatic patients is the definitive electrical stimulation.
Tachycardias by accessory pathways. Preexitation Syndromes. Wolf Parkinson and White syndrome
This syndrome characterized by paroxysmal episodes of supraventricular tachycardias in young patients was described in 1930 by Louis Wolf, John Parkinson and Paul D White.
Typical delta wave presence
It is characterized by occurring in adolescents and young adults, with repeated episodes of paroxysmal supreventricular tachyarrhythmias, its incidence varies between 0.6 and 4.8 per thousand.
The anatomical bases that determine these arrhythmias even given by the presence of bundles of myocardial fibers that determine in Wolf Parkinson and White syndrome, is characterized by presenting the so-called delta wave, which connects the atria with the ventricles, these bundles settle in any sector of the right and left atrioventricular valve rings and in the septal region, and can be single or multiple. These muscle fibers are not subject to the electrophysiological characteristics of the AV node, which is why they favor the reentry mechanism. When the pre-excitation activates most of the myocardium, the electrocardiographic diagnosis is easier, when the pre-excitation is of small magnitude, its diagnosis becomes difficult and sometimes impossible.
Numerous algorithms have been developed for the anatomical location of these abnormal pathways, which we consider to be familiar to the specialist cardiologist and electrophysiologists. It should be noted that on multiple occasions its location can only be achieved only in the electrophysiology laboratory, and we call them hidden pathways.
The paroxysmal supreventricular tachycardias are the most frequent arrhythmias and 2 varieties are recognized, the orthodromic variety in which the impulse descends through the normal pathway and returns to the atrium through the retrograde accessory pathway, and the antidromic variety in which it descends through the accessory pathway and returns. by the normal route.
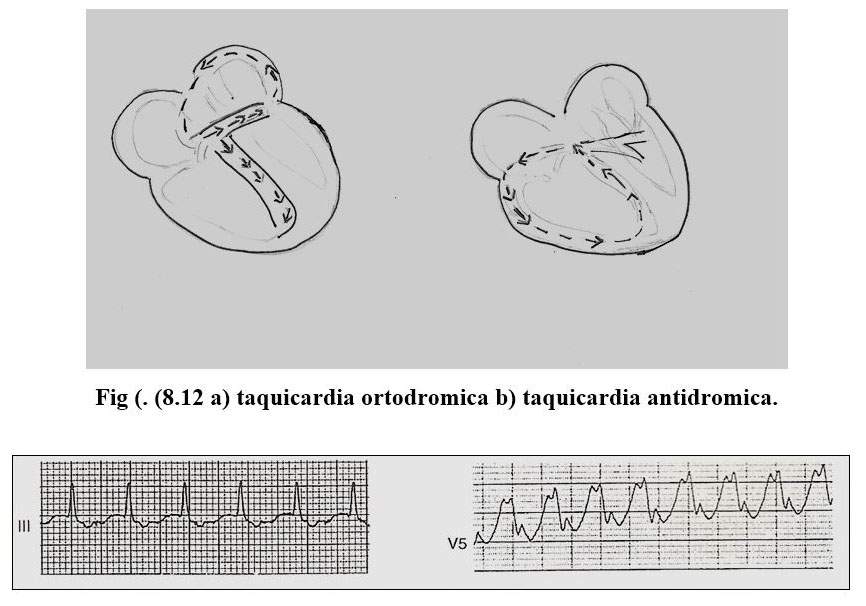
The orthodromic variety is characterized by narrow QRS and the P waves are inscribed behind the QRS complexes (RP shorter than the RP) and their frequency ranges between 150 and 250. Tachycardias are triggered by premature atrial impulses that find the accessory pathway refractory, they are conducted through the AV node, and return upon finding the abnormal pathway in the conductivity period, to the atria, restarting the circular motion again.
Paroxysmal antidromic tachycardia is less frequent in this case, the anterograde branch, that is, which leads the impulse to the ventricle, is the accessory pathway and the retrograde is the normal conduction system, in this case the QRS complexes are wide branch block type initially conducted by the ventricular myocardium and its heart rate is above 250 x 'the P waves are generally within the very wide QRS or T waves.
The incidence of AF and atrial flutter in WPW syndrome varies between 21% and 55%, according to different statistics, it presents in a paroxysmal rather than persistent or permanent form and its electrocardiographic pattern presents very irregular RRs that can be pseudonormalized when the frequency is very fast and QRS vary on occasions because ventricular activation can come from the normal conduction pathway or the accessory pathway; sometimes if the frequency is very high it can be confused with ventricular tachycardia. Its presentation is an indicator of risk, to develop sudden death, due to its high frequency.
Ventricular preexcitation explains 3.6% of sudden deaths in young people, and in 40% of cases they are not preceded by symptoms. Current advances in electrophysiology have allowed radiofrequency ablation of abnormal pathways to be the definitive solution for these patients today.
VENTRICULAR ARRHYTHMIAS
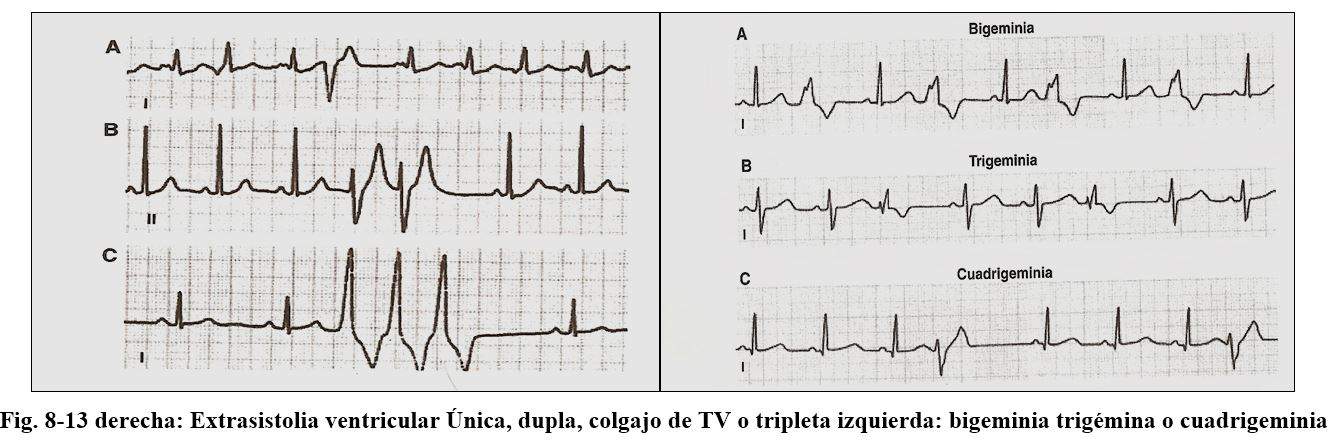
EXTRASISTOLIA VENTRICULAR
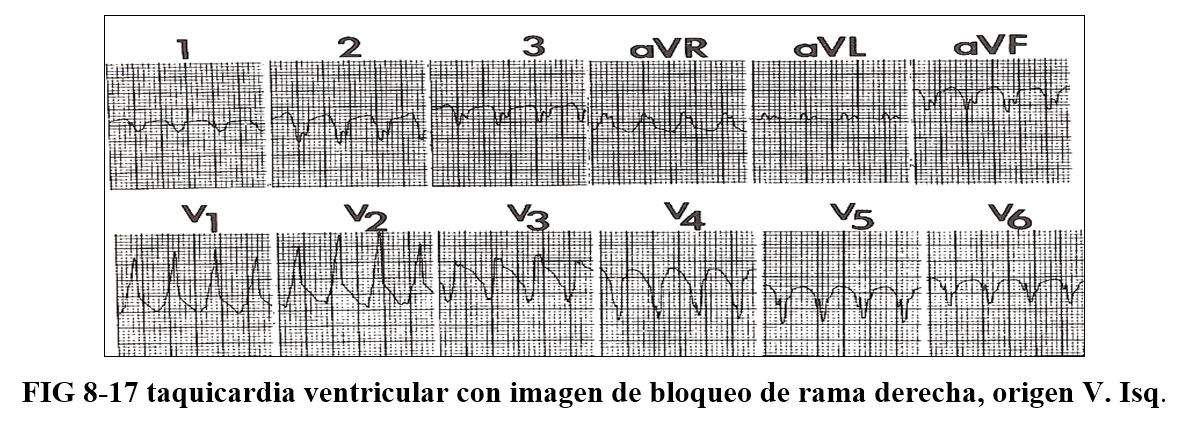
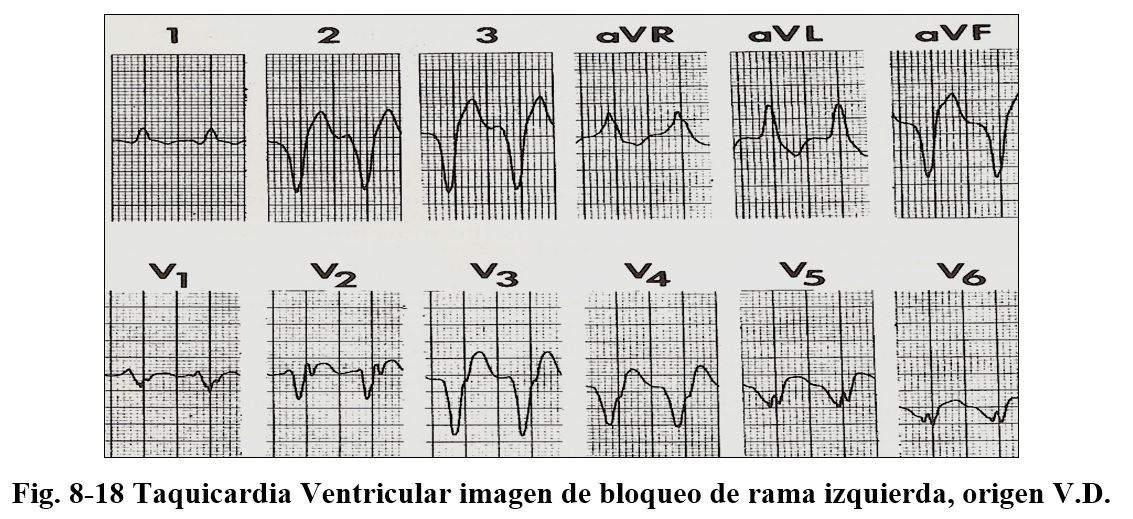
They are beats that originate anywhere in the conduction system below the bifurcation of the bundle of Hiss. The extrasystoles that come from
Left ventricle produces images of right bundle branch block, and those originating in the right ventricle have images of left bundle branch block.
They can originate in one of the branches of the Hiss bundle or in the Purkinje system, or in the ventricular myocardium.
The ECG shows the following patents: those that are from the left ventricle have a typical image of right bundle branch block and those that originate from the right ventricle have an image of left bundle branch block.
Extrasystoles can be monomorphic, bimorphic or polymorphic, depending on their site of origin. The ligation or coupling interval is the interval that separates it from the preceding sinus stimulus, when the arrhythmia mechanism is by reentry, its coupling interval is fixed, when the mechanism is not reentry, the coupling interval varies and is sometimes very short, originating the R / T phenomenon that in the context of ischemia or acute infarction can trigger sustained ventricular arrhythmia.
Lenticular beats can occur in duples (2 extrasystoles in a row or triples (sequence of 3 extrasystoles or ventricular tachycardia.
The p wave that follows a premature beat can be sinus and located earlier within the QRS or posteriorly in the ST segment. They generally present a complete compensatory pause, that is, the sum of the interval between the QRS preceding the extrasystole the extrasystole and the following sinus beat is equal to the length of two normal sinus cycles
Escape beats
They are called thus to one or more impulses that arise from different foci as a consequence of delay in the base rhythm
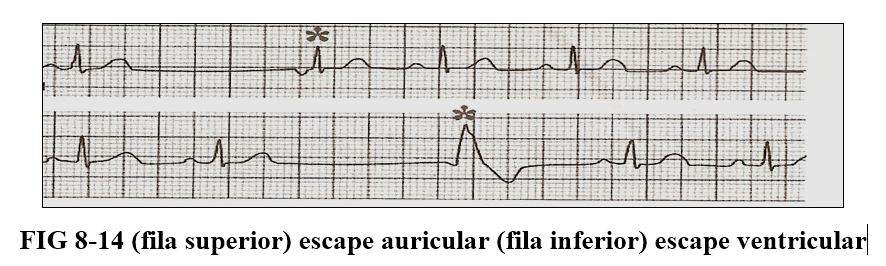
It can give rise to a rhythm that depends on the area where it originates from being, atrial, from the narrow ventricular or idioventricular AV junction, its frequency varies between 40 and 80 in the atrial, 35 to 60 in the junction and between 20 to 40 the which originate from the Purkinje network. (Fig. 8-11)
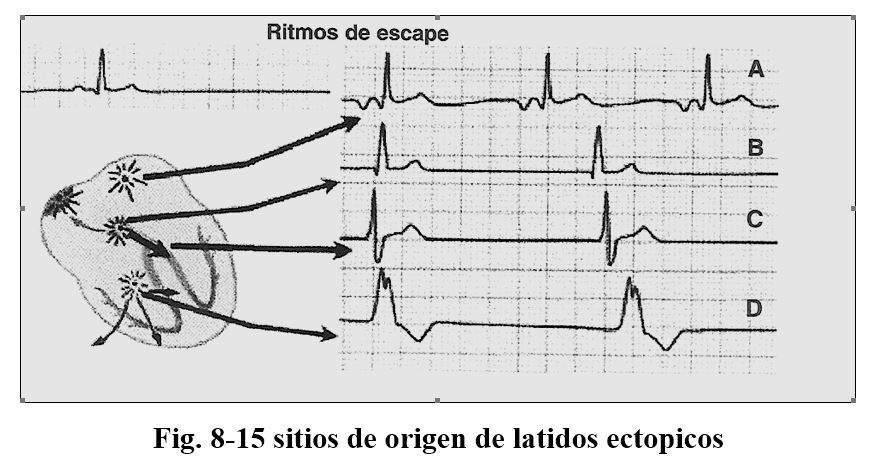
The ectopic atrial rhythm is characterized by presenting negative P waves generally in the D2 D3 AVF leads and they speak of a caudal origin.
The rhythms of the AV junction are characterized by narrow Qrs complexes with P waves that precede, register at the same time or follow the QRS, if they are visible they are always negative. The idioventricular rhythm is revealed when there is a depression of the sinus node or by the presence of AV-type blocks, they are narrow if they originate in the Hiss or in the beginning of the divisions of the branches and wide when they originate more distally.
The accelerated idioventricular rhythm is externalized when there is an increased automatism, which competes with the sinus rhythm.
VENTRICULAR TACHYCARDIA
We call ventricular tachycardia the sequence of 3 or more successive ventricular beats. They can be divided into sustained ones when they last more than 30 seconds or have more than 25 beats, and non-sustained ones are self-limited ones that do not meet these requirements.
There are diagnostic criteria to differentiate ventricular tachycardias from supperventricular with wide QRS:
a) QRS duration greater than or equal to 0.14 sec.
b) AQRS between -30º and - 90º or between - 90º and 180º
c) AV dissociation
d) presence of fusion and capture beats.
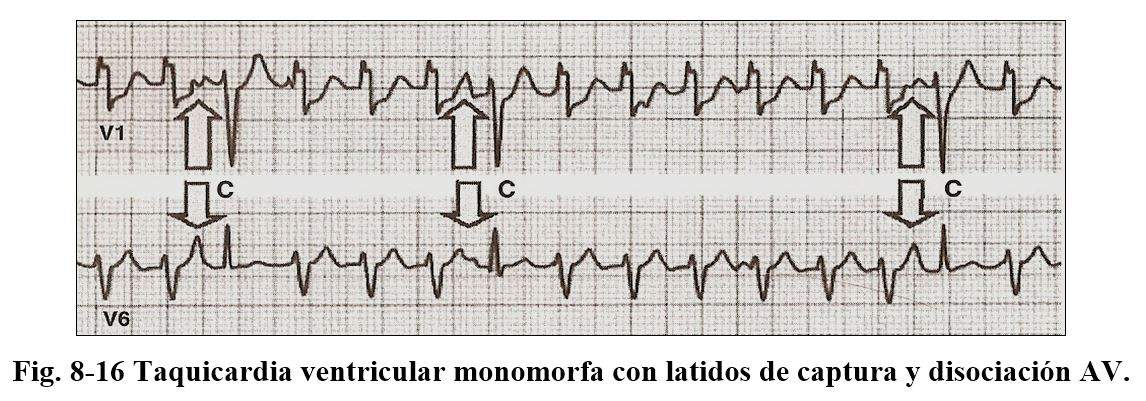
The presence of concordant QRS complexes, whether positive or negative in precordial, the absence of R / S complexes in precordial or without, the duration from the beginning of the R to the nadir of S measures more than 100 sec. certify the diagnosis of monomorphic TV.
In the presence of a tachycardia with an image of right bundle branch block we must take into account in V1 the presence of qR, QR, Rs, monophasic or triphasic complexes type Rsr ', or Rr' and in V5 morphology rS, QS, QR, or R, which indicate its ventricular origin.
When there is an image of left bundle branch block, the duration of R is greater than 30 msec. , interval between the start of R and nadir of S greater than 60 msec and presence of fillings in the S branch, together with the presence of q in V6.
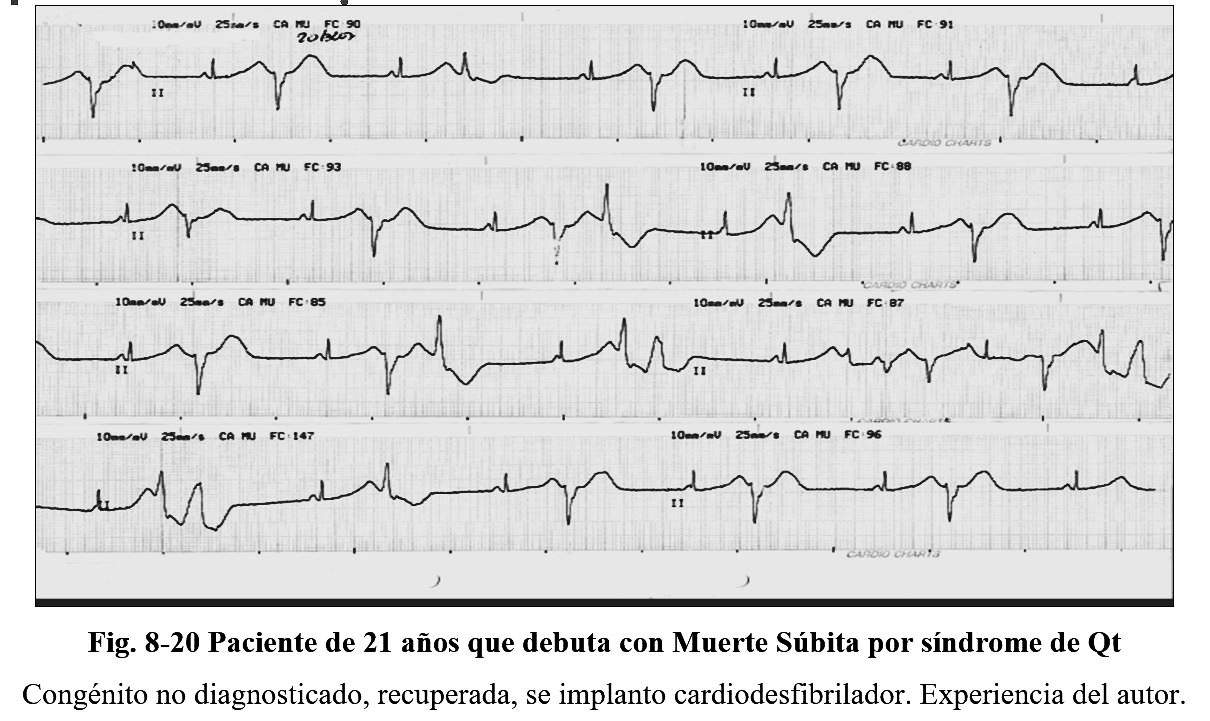
Polymorphic ventricular tachycardias are those that occur in prolonged QT syndromes, hereditary, or secondary to the administration of drugs in Brugada syndromes in catecholaminergic origin and in patients with coronary heart disease.
It is characterized in that the QRS complexes permanently vary in their amplitude, polarity, and configuration and generate a ripple around the isoelectric line, it presents a ligature of the beat that initiates the long arrhythmia and the RR intervals are irregular.
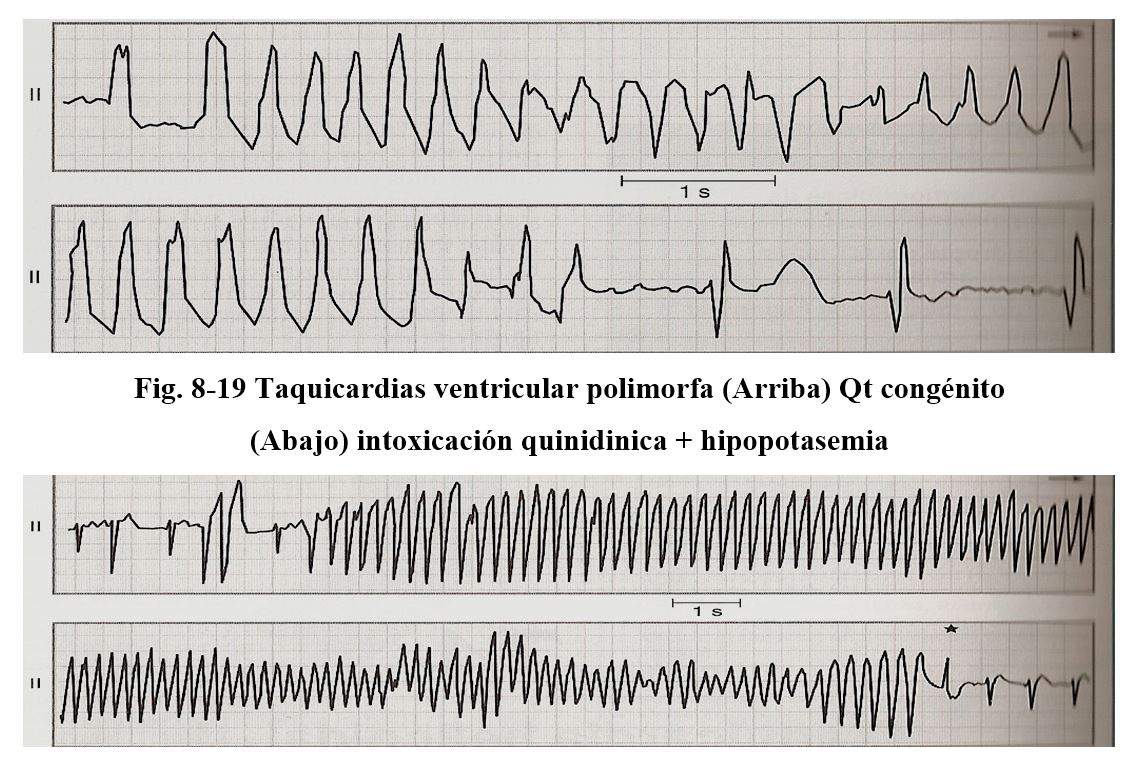
The frequency of these tachycardias is around 200 beats per minute, although they are self-limited, they frequently transform into ventricular fibrillation.
The mechanism would be conditioned by the reentry mechanism. Normal Qt is always less than 0.44, it is considered to limit up to 0.46 and prolonged when it is greater than these values. To determine the Qt, the Bazett formula is used (QTC = QT by the square root of the RR intervals.)
There are numerous drugs that can cause an increase in Qt quinidine, prenylamine, bepridil, phenothizines, tricyclic antidepressants, high concentrations of fluoxetine, and antibiotics such as ampicillin, erythromycin, clarithromycin, associations such as trimethoprim sulfamethoxazo, antihistamines such as terfenadine, etc. Within the water and electrolyte disorders, hypokalaemia and hypomagnesemia are also causes of these types of arrhythmia.
In congenital syndromes, there are protein abnormalities in the sodium and potassium channels and numerous variants have been described by Jervell, Lange Nielsenn; From Romano Ward and within this, 7 different mutations have been identified, identified as LQt1 to LQt 7.
Catecholaminergic tachycardias are hereditary in nature, and are related to physical or mental stress.
Brugada syndrome is a congenital disorder characterized by the patient presenting episodes of polymorphic ventricular tachycardias. The genetic alteration is of autosomal dominant transmission that is located on chromosome 3 and specifically affects the sodium channel, some alterations are reading errors others are alterations in intron 7 and the last one affects the SCN5A gene, inhibition of the channels would occur of sodium during phase 1 of the action potential, as a consequence the potassium output current is not followed by sodium input, generating a shortening of the action potential. These facts become evident with the increase in body temperature.
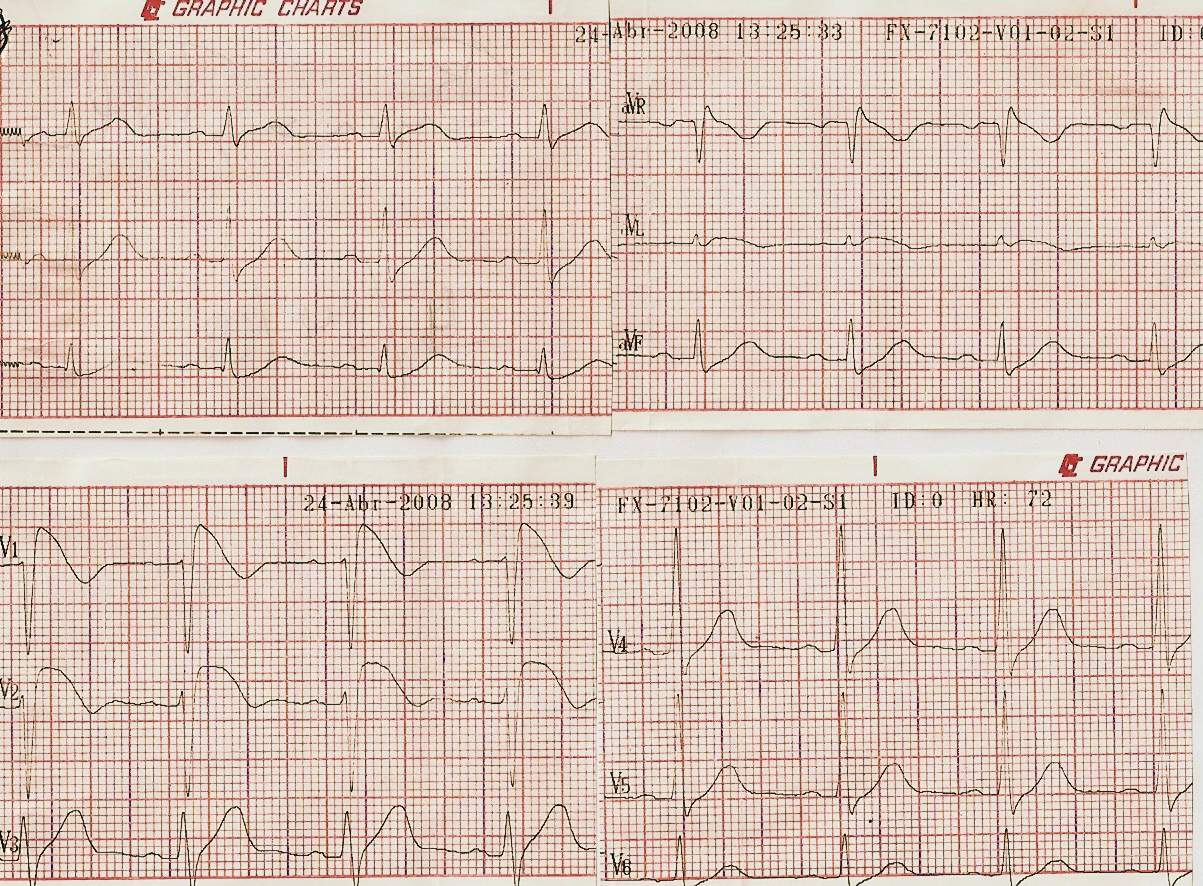
Fig 8-21 Brugada syndrome
The ECCG is characterized by presenting an image of RBBB predominantly in leads V1 and V2 with elevated ST in the saddle image. Sometimes the variations are not very typical and can be evidenced as seen in Fig. 8-21 with the administration of ajmaline, procainamide or flecainide, in this case 800mgrs of flecainide was used.
Its finding can be accidental and the electrocardiographic patterns can be found in routine examinations. In patients with a typical pattern on the ECG and resuscitated episodes of sudden death, the indication is the placement of a cardioverter defibrillator. The behavior is more complex when there are no typical patterns and in totally asymptomatic patients. To take the behaviors in these patients, the patient's family history should be considered, that is, a history of sudden death, and their age, since the highest incidence of malignant arrhythmias occurs around the third to fourth decade of life.
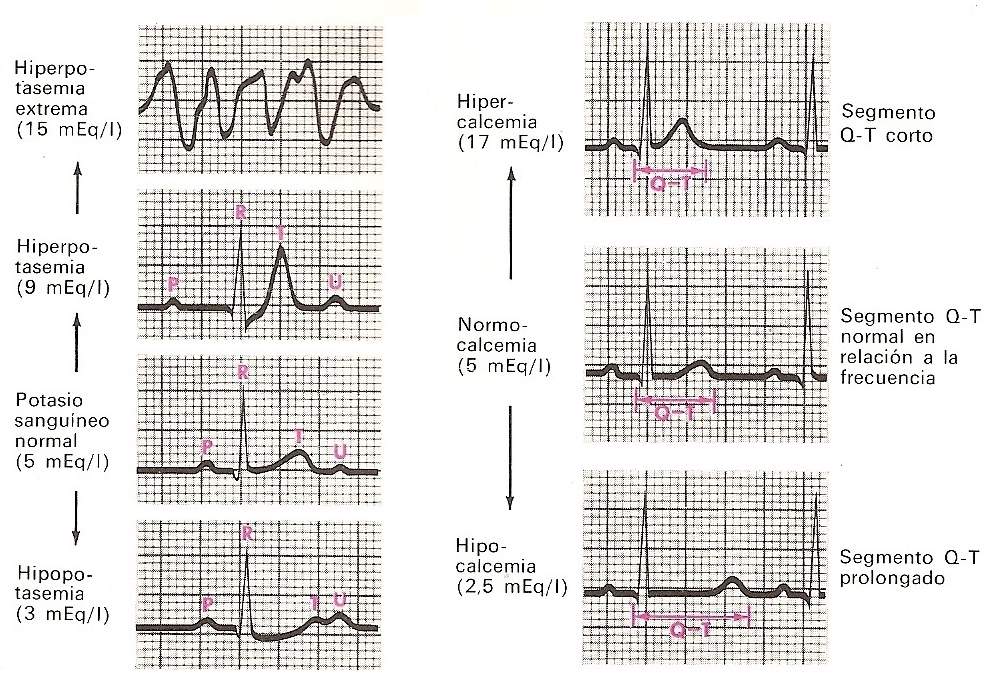
Hydroelectrolyte Disorders
Potassium and calcium are the electrolytes that have the greatest importance in cardiac functioning and their variations cause electrocardiographic alterations.
Hyperkalemia depresses the atria, the Av node and the ventricles with less effect on the sinus node, its increase causes prolonged PR intervals and high T waves, sinoatrial block, with absent contractions of the atria, presence of tent t waves, widening of the QRS and finally ventricular fibrillation or cardiac arrest.
Hypokalemia causes loss of T wave amplitude, prominences of U waves with greatly increased Qt intervals.
Hypercalcemia is characterized by shortening of the Qt interval, and hypocalcemia increases the duration of the sf and Qt intervals.
Semiological diagnosis of arrhythmias
The diagnosis of arrhythmias at the bedside continues to be of great importance despite the many advances in medicine in the field of cardiology
Without a doubt, the electrocardiograph is the most important auxiliary for the diagnosis of arrhythmias; but sometimes it is not available and it is for this reason that all possible knowledge should be used for its diagnosis. For this, it is necessary to pay attention to the various clinical and semiological findings, the combination of which often leads to a correct diagnosis.
Tachycardias represent frequent reasons for consultation, which the patient refers to as "noticing that his heart is at times very fast", sometimes referring to it as working even or unevenly, of variable duration, sometimes being seconds, minutes or hours. Sometimes it is accompanied by various symptoms such as polyuria, desire for defecation, sweating, paleness, dizziness or hypotension. The questioning should examine whether the tachycardia is regular or irregular and if it is related to efforts or if its presentation is at rest. .
Normal sinus tachycardia
In normal sinus tachycardia, conduction from the sinus node to the ventricles differs only in rate. The range of variation of this is highly variable, considering that we consider tachycardia when the frequency is greater than 100 x '. It can appear as a consequence of multiple physiological causes, exercise, emotional states or secondary to excessive drinks, coffee, cigarettes, drugs such as atropine, ephedrine or febrile states, anemia, hyperthyroidism.
The rate may be accelerated when associated with significant hypotension, shock, or bleeding. Faster heart rates are normal in children, usually on the order of 120 beats per minute, although occasionally in infants they may have rates of 180 to 200 x '. After the age of 13, the heart rate tends to decrease.
Basis for the diagnosis: In normal sinus tachycardia, the rhythm is essentially regular and remains constant, except for small variations that normally occur with respiratory changes. The first heart sound is generally accentuated, and pacing of the carotid sinus produces a gradual rate delay followed by a return to the previous rate upon cessation of compression.
Paroxysmal atrial tachycardia
This tachycardia, as its name expresses it, is of sudden onset, it can last a few seconds, minutes or persist for days, sometimes it is incessant, that is to say that the patient is permanently in tachycardia.
The sudden regular and rapid onset is accompanied by frequencies between 150 and 250 beats per minute, it appears more often in individuals who do not have another manifestation of organic heart disease and its presentation is not related to any particular event, even though in some individuals It can be linked to emotional states, rough exercises, or certain rapid movements of the body.
The patient describes these as “fluttering or tapping” and can sometimes identify them by observing the doctor's hand to imitate rapid and regular movement over his precordial region.
In some patients, they can present for years sporadically without determining alterations, while in others it can evolve to tachymocardiopathy when its presentation is more frequent and prolonged.
In a pathological heart it can determine cardiac decompensation, or the presence of anginal pain or even myocardial infarctions, in some patients blood pressure drops and pulse pressure is markedly reduced. In patients with coronary artery disease, typical chest pain can be seen coinciding with the rapid ventricular rate. Polyuria can accompany the episodes. As far as possible, the doctor should examine the patient in paroxysms and try to document it electrocardiographically in order to confirm the diagnosis its probable formation mechanism and the intervention of anomalous preexitation pathways. In children, the presence of vomiting accompanying irritability, increased respiratory rate and sometimes cardiomegaly and hepatomegaly is frequent.
Basis for diagnosis: Regular rhythm, irregularity is reason to look for another type of arrhythmia.
First Noise increased with slight respiratory variations.
Carotid sinus compression. This maneuver, carried out correctly, is of great importance for diagnosis and treatment, as it can cause the sudden termination of the arrhythmia.
Compression of the carotid sinus: the patient must be placed in supine position, with the head lateralized to the left side and the doctor must palpate the beat of the carotid artery in its bifurcation below the angle of the maxilla, and should not be performed if it is not possible. palpate the artery, since it is sometimes a painful maneuver, and the patient should be auscultated while performing it. In case of being ineffective, it can be tried on the opposite side, the pressure exerted on the breast must be sustained and not more than 4 seconds, loosening and re-exerting it later, doing it together as a massage movement to be effective.
There are other methods or tricks to achieve a vagal effect, these are: the valsalva maneuver that consists of taking a deep inspiration and without expelling the air, making force with the mouth closed to expel it, or as if by tensing the abdominal muscles, while performing the carotid compression.
Sometimes the patient learns maneuvers to cut the tachycardia: the Valsalva maneuver, lying across the bed with the head tilted to the ground, or bending over and placing the head between the legs while performing the Valsalva maneuver. Other procedures that can be effective are, causing nausea or vomiting by resting 2 fingers on the base of the tongue, ingesting ice water or placing ice on both eyelids.
Compression of the eyeballs is sometimes effective, although it generally fails because of the doctor's fear of causing injury to the eyes or because it is also a painful maneuver.
It is convenient while performing these maneuvers to record the electrocardiogram, to show the changes that could be achieved. Many times these are not effective and it is necessary to medicate, to achieve the reversal of the arrhythmia.
Atrial fibrillation
It is one of the most common and frequent tachycardias. In general, this tachycardia is not difficult to recognize at the bedside, due to its irregular and rapid heart rate. Its frequency varies between 100 and 200 beats per minute, it is observed in states such as rheumatic valve disease, mitral stenosis, mitral regurgitation, hypertensive heart disease, ischemic heart disease, myocarditis, thyrotoxicosis, in patients with infectious symptoms such as lung disease, or in people without clinical expression of heart disease.
Basis for diagnosis: First heart sound. Its intensity varies from slight to considerably increased and together with a totally irregular rhythm are characteristic data. In valve pathologies with mitral stenosis, this first noise will be heard, totally increased in intensity, in severe mitral regurgitation it is diminished in intensity.
Carotid sinus compression: during this maneuver there is a slowdown in its rate, but there is no reversal of the arrhythma to regular sinus rhythm and upon cessation of compression, a gradual return to the previous rate is observed.
Venous pulse: jugular engorgement is observed without collapse and on some occasions the presence of slight oscillations.
Its early diagnosis is of vital importance to institute early treatment and avoid complications in high-risk patients.
Atrial fibrillation can be classified as: Recent acute AF of less than 48 hours. presenting, recurrent AF, paroxysmal AF, and persistent AF.
Regarding the risks of producing embolisms:
High risk: a history of fixed or transitory stroke, over 75 years of age associated with hypertension, diabetes or vascular disease, valvular heart disease or deterioration of ventricular function.
Moderate risk: age over 65 without risk factors or over 75 with hypertension, diabetes or vascular disease.
Low risk: under 65 years without risk factors.
According to the risk of each patient, the corresponding strategy will be taken for the management and indication of anticoagulation or preventive antiaggregation.
Atrial flutter
In this arrhythmia the atria beat at a rate of 250 to 350 per minute, but not all stimuli are conducted to the ventricles. At the AV node level, the physiological delay occurs, which determines a 2: 1 or 4: 1 delay and, based on the degree of blockage, it will be the frequency.
Its form of presentation and accompanying symptoms do not vary from the previously mentioned tachycardias, as do the determining causes.
The diagnosis of flutter is unlikely to be performed at the bedside without having an electrocardiographic record.
Basis for the diagnosis: regular rhythm, a reason that makes it difficult to differentiate, but a certain degree of irregularity may occur.
First constant noise does not vary in intensity.
Carotid compression: a decrease is observed with compression, with a subsequent return to the previous rate without reversal of the arrhythmia. In patients with sinus dysfunction, the return to the previous rate may be slower and during the compression phase the degree of blockage is very evident, producing prolonged asystoles, which is why we advise in elderly patients not to perform it without electrocardiographic monitoring.
Venous pulse: you can see small irregularities (small and fast “a” waves)
Ventricular tachycardia
It is one of the most serious arrhythmias, and its presence always indicates the presence of a severe underlying heart disease. The presence of structural heart disease and its ejection fraction will determine the hemodynamic status and the patient's presentation.
If you have a low ejection fraction, your tolerance status will be very bad, presenting signs of low cardiac output, hypotension, profuse sweating, until you reach syncope, if your cardiac involvement is not severe, your tolerance will be greater, until you reach no be almost perceived.
Basis for the diagnosis: First heart sound: it is characteristic that it changes intensity; at times it is strong and at other times weak, and is associated with the change in the PR relationship in the sense that they are dissociated in their sequence. The variation in its intensity is a valuable parameter for its diagnosis.
Carotid sinus compression: not effective for ventricular tachycardia.
Ventricular fibrillation
In this arrhythmia, which is generally fatal, no effective contraction of the ventricles occurs, but rather undulating movements occur after cardiac contraction has ceased. Circulation is interrupted and death ensues shortly after, otherwise resuscitation maneuvers are instituted.
Heart blocks
First-degree block: the diagnosis of this type of block is generally made through the electrocardiogram, but there are semiological data that cannot approach the diagnosis. It is carried out through the auscultation of the first noise, as the PR shortens to values of 0.10 to 0.14 the intensity of the first noise increases and when the PR lengthens, it decreases in intensity. The presence of a first noise diminished with a second normal noise suggests the possibility of this blockage.
Second-degree block: its symptoms are determined by the heart rate that determines the block. Sometimes the sudden decrease in the frequency can be perceived as a sensation of cardiac arrest, causing a sensation of dizziness, variable palpitations until syncope.
Bases for the diagnosis: Rhythm is changing, which means that from a frequency of 80 beats per minute it can fall to a frequency of 40 beats per minute, it is in those moments, the symptoms appear.
Frequency: On auscultation, a slow ventricular rate is perceived and the presence of an easily detectable atrial noise or fourth noise, as it appears and disappears during auscultation and its origin is determined by a more intense atrial contraction that occurs in the filling phase. against a less compliant ventricle.
Third degree block or complete AV block: in this arrhythmia the atrial and ventricular contractions are totally independent and the diagnosis can be confirmed by paying attention to some signs.
Basis for the diagnosis: First noise: it varies in intensity and in diastole weak atrial sounds can be heard. These extra contractions can be felt in the pulse.
Jugular venous pulse, atrial waves can be observed during the long pauses with the presence of cannon waves that are produced when the atria contract with the AV leaflets closed, coinciding with ventricular systole. Another important semiological data is the variable character in the intensity of the first noise, its increase is determined by the late closure of the valves, that is, very close to the rise in pressure in the left ventricle.
The presence of a slow heart rate between 45 and 50 beats per minute raises the differential diagnosis between complete second-degree AV block or normal sinus bradycardia. If the frequency is 44 per regular minute and the presence of atrial noises as well as cannon or accessory waves in the venous pulse and the lack of increased heart rate can be perceived; the diagnosis of complete AV block is imposed.
It should be remembered that in the case of suspected AV block, compression of the carotid sinus should not be performed.
Branch blocks.
Right bundle branch block can be diagnosed by the existence of a second split noise, this splitting is due to the delay in electrical activation of the right side of the heart, which persists during expiration.
In left bundle branch block, the second heart sound may present a narrower splitting or be unique on inspiration and wider on expiration, taking the name of “paradoxical” splitting.
Extrasystole
Its presence is frequent in the examination of patients and a priori should not be considered pathological.
These may or may not be symptomatic and sometimes the patient describes them as his heart "jumping" or as a sensation of a "bubble that rises". Other times they can be referred to as "the heart stops" (due to the perception of the extrasystole pause) and be accompanied by a coughing fit.
The triggering causes of extrasitolia are diverse, coronary heart disease, hypertensive, valvular heart disease, cardiomyopathy, and general conditions such as infections, sepsis, thyrotoxicosis, even functional states, stress, medications, drugs, excess coffee, cigarette, alcohol, etc.
The presence of all arrhythmia has a different prognostic value when accompanied by processes with severe depression of cardiac function, such as ischemic or idiopathic cardiomyopathy.
On auscultating the heart, it is noted that the regular rhythm is abruptly interrupted by an extrasystole followed by a pause. In ventricular extrasystole the pause is compensatory (two beats including extrasystole is equal in duration to two normal cycles) in atrial the pause may not be compensatory. The extrasystoles can be perceived when palpating the pulse and in the observation of the jugular pulse, in numerous occasions it is the patient who notices them when registering his own pulse.