Fernando L. Soldano, Dr. Antonio Molina Rojas and Dr. Gustavo Lavenia
Acute renal failure (ARF), acute renal failure or failure is a clinical syndrome, secondary to multiple etiologies, characterized by a sudden deterioration of renal function that occurs in a period of a few hours to days. The common expression is always an increase in the concentration of nitrogenous products in the blood (uremia and creatininemia). Around 60% of cases present with oliguria (diuresis less than 400 ml / day in adults). You can also do it with a higher diuresis, even higher than 2 liters. Therefore, it is important not to overstate the diagnostic value of urine volume.
Three premises are necessary for renal function: adequate blood perfusion, integrity of the renal parenchyma, and permeability of the excretory pathways. The sudden alteration of any of these elements can cause the deterioration of the renal function. Depending on the altered functional element, ARF will be classified as A - pre-renal: if the main alteration is the failure of renal perfusion; B - renal, parenchymal or intrinsic: if the alteration lies in the renal structures and C - post-renal or obstructive, if the urinary flow is interrupted.
Epidemiology
The etiology and incidence of ARF depend fundamentally on the geographical-economic aspect and the area where it occurs. Its incidence in Europe is between 200 cpm / year / adults and 30 cpm / year / children. ARF is seen more frequently in men (66%), being more frequent in people over 60 years of age, but it can be seen at any age. It occurs both in the hospital environment (60 percent) and out-of-hospital. Etiologically, diagnosed out-of-hospital ARFs are mainly due to obstructive conditions of the urinary tract, dehydration, and renal parenchymal diseases (glomerulonephritis, vasculitis, etc.), while in-hospital ARIs are usually tubular necrosis, generally secondary to therapeutic and diagnostic techniques (surgery, drugs and iodinated contrasts).
|
Etiology of acute renal failure
|
IRA Clinic
Symptoms related to functional impairment and symptoms of the originating process may occur. Due to this, the clinical presentation is extremely variable and depends in part on the severity of the ARF. The picture can vary between polyuria, with mild manifestations, and oligoanuria, which is more symptomatic. If there is anuria (diuresis less than 100 ml / day) it may suggest the existence of bilateral obstruction of the renal arteries, bilateral cortical necrosis, bilateral medullary necrosis, bilateral papillary necrosis or bilateral obstruction of the ureters (lower urinary tract pathology). The normal value of uremia (15-35 mg / dl) will increase in direct proportion to the catabolic status, in hypercatabolic patients (infections, severe trauma, burns, shock, incompatible transfusions) can exceed 100 mg / dl / day). Creatininemia (VN = 0.8-1.2 mg / dl) will rise proportionally to uremia in Parenchymal and Obstructive ARF pictures. In Prerenal ARF, in its initial phase the 30/1 (Ur / Cr) ratio, normally present, is altered, initially increasing Uremia, breaking this relationship. In its evolutionary phase, if the original picture is not resolved, it will equalize following this relationship. Normally, the formation of non-volatile acids, a product of protein catabolism, are eliminated by the kidney, there will be retention of them, with a decrease in serum bicarbonate in proportion to catabolic status, being between 1 to 2 mEq / day and higher in hypercatabolic . It can present cardiovascular alterations such as Arterial Hypertension and Heart Failure due to hydrosaline retention. The intake and excessive fluid intake can produce intoxication due to excess free water, causing neurological symptoms such as altered level of consciousness, from confusion to coma and convulsions, due to hyponatremia and cerebral edema. Potassium also increases by cellular catabolism, presenting according to its serum level, from ventricular and supraventricular arrhythmias, and in severe cases, by association with acidosis and hypocalcemia, cardiac arrest and death of the patient. Other laboratory findings include leukocytosis, with or without associated infections and the presence of coagulation abnormalities. If the signs and symptoms described are severe, replacement treatment of renal function with dialysis may be required (see Chronic Renal Insufficiency). If substitution treatment is not required, It can present recovery of the diuretic rhythm in oligoanuric forms, which can take from hours to weeks, reaching normality. Frequently in these cases, they present recovery polyuria, and they should be attentive to the hydrosaline balance, since they can present massive diuresis with cardiovascular collapse. Despite these events, uremia and creatininemia may continue to be high and after days, begin to decrease.
In non-oligoanuric ARF, 40 to 80% of patients present with normal urinary volumes and even polyuria. The most common causes of non-oligoanuric ARF are aminoglycosides (especially gentamicin), radiographic contrast agents (iodine), methoxyfluorane, severe burns, severe multiple trauma, surgical causes (especially with extracorporeal circulation), and non-rhabdomyolysis. traumatic. In this form of ARF, urinary sodium is lower than in oligoanuric, they have a shorter hospitalization time and fewer episodes of complications (infectious, hemorrhagic, neurological disorders and less acidemia). These patients have a lower replacement requirement for renal function, which reduces mortality to 25%, while in oliguric forms it is around 50%.
Complementary Studies for Diagnosis
It should be evaluated:
-
Is it an acute or chronic disorder?: In ARF, creatinine rises at least 0.5 mg / dl / day, in CRF the nitrogenous products remain constant. The existence or presence of a history of kidney disease or uremic syndrome (asthenia, anorexia, somnolence, cramps, nausea, vomiting, polyuria or long-standing polydipsia), as well as hypocalcemia, hyperphosphataemia, well-tolerated anemia, hyperkalemia and hyperchloremic acidosis , suggest CRI, but do not rule out ARF or flare-up of CRI.
-
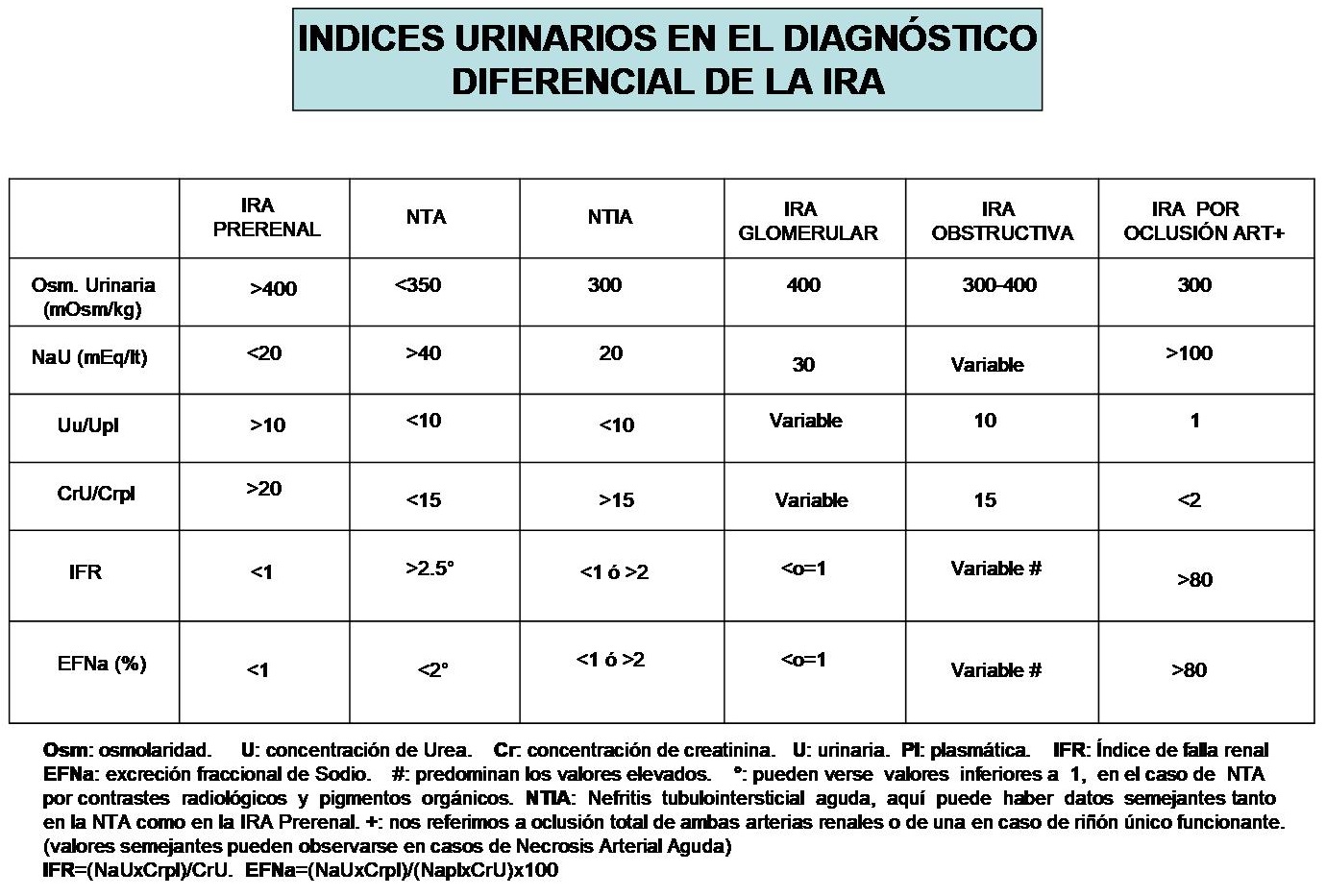
Rule out urinary tract obstruction: the clinical history (history of renal colic, hematuria, trauma, gout, prostatism, abdominal and pelvic neoplasms, and aortic aneurysms), and abdominal ultrasound (kidney, bladder and prostate) and gynecological, will provide us with information on renal size and morphology, prostate size, presence of bladder balloon, signs suggestive of urinary tract dilation, and direct and indirect findings of lithiasis. The ultrasound evidence of small kidneys is typical of CRF, normal or large kidneys are more frequent in ARF, but it does not imply a definitive diagnosis, since, in pathologies such as Diabetes, Amyloidosis and Polycystic Kidney, causes of CRF, these they are usually normal or enlarged in size. This is the first step in the examination that should be performed in all patients with impaired kidney function. If this method is not available, a simple abdominal X-ray can diagnose radiopaque lithiasis, but its negativity does not exclude radiolucent ones. A history of extracorporeal losses (bleeding, diarrhea, diuretics), redistribution of ECL (gastrointestinal entrapment, pancreatitis, rhabdomyolysis and edema), or clinical signs of renal hypoperfusion (shock and heart failure) initially suggest a prerenal origin of ARF. The clinical examination will reveal hypotension, tachycardia, ocular hypotonia, crease sign, and dry mucosa frequently. However, its absence does not rule out LEC depletion. The presence of ascites, jaundice, liver stigmata and / or edema, suggest a hepatic origin of the decrease in circulating volume responsible for renal failure. The existence of severe valvular heart disease, especially left, an AMI or other causes of Heart Failure, will guide us to the cardiac origin of Prerenal ARF. Among the causes of shock (sepsis, aortic dissection, adrenal or pituitary insufficiency and acute heart disease) result in a Prerenal ARF. Due to its functional nature, Prerenal ARF improves when the original cause does. For this reason, when pure hydrosaline depletion is suspected, it must be improved with volumetric expansion, using 1 to 2 liters of IV fluids at a rapid rate, but according to cardiac sufficiency and the age of the patient. The use of pressor drugs with varying degrees of volume expansion should be considered. In elderly patients, With cases of shock and cardiopathies, invasive hemodynamic monitoring with catheters for measurement of Capillary Venous Pressure (PVC) or use of a Swan-Ganz catheter for measurement of Pulmonary Capillary Venous Pressure (PVCP) is advisable. The corrective response of these processes and the improvement of urinary output with them, point to a prerenal origin. If they do not improve, they point to an ATN of ischemic origin. The determination of analytical tests of blood and urine constitute the pillars in the differential diagnosis of ARF, especially in 3 situations: Prerenal ARF, ATN and the total occlusion of the renal arteries. Diuretic doses should not be taken until the composition of the urine has been analyzed, since their use modifies the composition of urinary electrolytes. The fractional excretion of Sodium (EFNa) is the most specific parameter. In general, values lower than 1 suggest a prerenal origin, while those higher than 3 are only seen in ATNs. Sometimes intermediate EFNa values between 1 and 3 can be seen in both situations, although it is more suggestive of NTA. In ARF by contrast media and pigments, the EFNA is usually less than 1. The following table shows the urinary indices for the differential diagnosis of ARF.
-
Is there evidence of vascular disease? The presence of anuria is a symptom of major and severe vascular compromise, although it is also present in bilateral obstruction. The use of ECO-Doppler provides information on renal arteries and veins, in addition to its use in the diagnosis of artery stenosis and renal vein thrombosis, it could be useful in the diagnosis of AKI due to ATN. In these cases, at the level of the interlobar arteries, there is an increase in resistance and a decrease in arterial flow, which revert with the resolution of the condition. Despite its diagnostic value, in cases of suspected acute arterial occlusion or renal thrombosis, conventional angiographic studies remain the technique of choice.
-
Findings suggestive of NTIA (Acute Tubulo-Interstitial Nephritis): having ruled out the hemodynamic etiology of ARF, a drug and / or toxic etiology must be considered, this requires an anamnesis referring above all to a recent performance of radiological examinations with contrast, use of medications (they can cause ARF due to kidney toxicity or hypersensitivity) and drug abuse. Mild proteinuria may be found.
-
Dermatological examination is important, eg. The presence of a morbilliform rash suggests NTIA, the presence of nodules, maculopapules, petechiae or facial erythema, a vasculitis or SLE. The presence of livedo-reticularis, an atheroembolic disease.
-
Regarding the urinary sediment, in ATN, only granular and / or hyaline casts, leukocyturia and microscopic hematuria are usually found. Heavier sediment (broad ARI casts) suggests other forms of Parenchymal ARI.
-
Renal Biopsy: indicated when the condition does not progress favorably in 3 weeks, because in this period 65% of ATNs progress favorably or should be performed earlier if another type of parenchymal ARF is suspected.
- Other determinations: serum complement dosage (C3, C4, CH50), cryoglobulins, Immunoelectrophoresis, ANCA (anti-neutrophil cytoplasm antibodies), Antinuclear antibodies and the practice of arteriography, renal scintigraphy with Gallium, complete the diagnostic tools.