Estrada Seminario Ronald Ricardo
This syndrome refers to the defective mucosal absorption of nutrients and poor digestion refers to their altered hydrolysis.
These terms differ from one another from the pathophysiological point of view, but clinically they manifest in the same way with signs and symptoms that express the inadequate assimilation of nutrients, vitamins and trace elements; which makes the clinical manifestations very diverse.
Pathophysiology
The integration of digestion and absorption includes:
- Luminal phase
- Mucosal phase
- Removal or Transportation Phase
-
Luminal Phase: In this phase, the fats, proteins and carbohydrates in the diet are hydrolyzed and solubilized by pancreatic and biliary secretion.
The pathophysiological mechanisms that come into play in this phase are three:-
Defective hydrolysis of nutrients:
- Lipase inactivation: in Zollinger-Ellison syndrome, acidic Ph prevents the activation of pancreatic lipase, selectively inhibiting fat digestion.
- Enzyme deficiency: in pancreatic insufficiency, the decrease in pancreatic proteases reduces the hydrolysis of proteins, this deficiency contributes to the loss of muscle mass and body weight.
- Inappropriate mixing or rapid transit: in intestinal resection, bypass, hyperthyroidism; In these cases, the hydrolytic enzymes lack sufficient time to complete the intraluminal digestion of carbohydrates.
-
Altered fat solubilization:
- Reduction of bile salt synthesis due to hepatocellular disease
- Impaired secretion of bile salts due to chronic cholestasis
- Inactivation of bile salts by bacterial overgrowth
- Impaired CCK (cholecystokinin) release from intestinal mucosa disease
- Increased losses of bile salts due to disease or resection of the terminal ilium
-
Lower availability of nutrients:
- Cofactor deficiency as in pernicious anemia or decreased functional surface area as in gastric surgery
- Nutrient consumption: bacterial overgrowth (Blind Handle syndrome) induces a decrease in the formation of micelles, which reduces the concentration of conjugated bile salts, manifesting clinically with steatorrhea (malabsorption of fats) and deficiency of fat-soluble vitamins.
-
Defective hydrolysis of nutrients:
-
Mucosa Phase:
- Extensive mucosal loss due to intestinal resection or infarction
-
Diffuse mucosal disease
- Gluten sensitivity: It is characterized by poor absorption of nutrients in the portion of the intestine that is damaged and a rapid clinical improvement after the exclusion of gluten from the diet.
- Crohn's disease: inflammatory, asymmetric, segmental, recurrent and chronic, transmural process that can affect from the mouth to the anus; but typically it affects the ilium, colon, or perianal region.
- Radiation Enteritis: Complication of antineoplastic treatment. High-energy X-rays or gamma rays produce ionization in tissues; molecules or atoms with sufficient electrical charge to cause injury in healthy cells.
- Whipple's disease: Rare systemic pathologies that when it affects the digestive system produces diarrhea, abdominal pain, weight loss and malabsorption; of infectious etiology (Tropheryma whippelii) that responds to adequate antibiotic treatment.
- AIDS Enteropathy: Enteric HIV infection leads to mucosal atrophy resulting in malabsorption with diarrhea and weight loss. A degeneration of nerve axons with destruction of endothelial cells was also demonstrated, leading to motor disorders including intestinal pseudo-obstruction.
- Amyloidosis: Malabsorption can be due to bacterial overgrowth, mucosal ischemia, exocrine pancreatic insufficiency or submucosal amyloid deposit that creates a physical barrier that prevents absorption.
- Sarcoidosis: The small intestine can be affected secondarily by the enlargement of the mesenteric lymph nodes; which can manifest with malabsorption accompanied by protein-losing enteropathy.
-
Enterocyte Defects
- Microvilli Inclusion Disease
- Hydrolase deficiency in the brush border; needed to hydrolyze disaccharides (lactase hydrolyzes lactose to produce glucose plus galactose)
- Transport defects (hartnup cystinuria; B12 and folate uptake)
- Epithelial processing: in A beta lipoproteinemia there is an alteration in the formation of chylomicrons
-
Removal or Transportation Phase
- Blood: vasculitis-atheromas
- Lymphatic: lymphangiectasia, radiation, tumor, or lymph node infiltration.
Chylomicron and lipoprotein absorption is hampered, resulting in poor fat absorption and protein-losing enteropathy.
Clinical picture
This great syndrome is made up of intestinal and extra-intestinal signs and symptoms.
In malabsorption syndrome, gastrointestinal symptoms vary from the simplest such as a slight increase in the frequency, volume or color of the stool to the typical steatorrhea, which is the elimination of abundant stool with a foul odor, grayish yellow or pale, soft and greasy that floats on water and sticks to the toilet; indicating poor fat absorption. In contrast, watery diarrhea accompanied by abdominal distension, borgorisms, and flatus indicates colonic fermentation of poorly absorbed carbohydrates.
Weight loss is another parameter that we have to evaluate, it is not the same to lose weight in a short time than to do it gradually and in a long time as occurs in malabsorption and also to relate it to the preservation of appetite or not.
The presence of gastrointestinal signs such as a space-occupying mass in the abdomen makes us think of Crohn's disease, lymphoma, TB, while distension points to intestinal obstruction, pancreatic pseudocyst ascites, motility disorders, the presence of steatorrhea forces the patient to doctor to rule out diseases of the mucosa, bacterial overgrowth, pancreatic diseases.
Extraintestinal signs are related to the lack of nutrients and trace elements in the different body systems:
-
Skin
- Paleness (severe anemia)
- Reduced subcutaneous fat
- Blisters, petechiae (Vitamin K deficiency)
-
Hair
- Alopecia (Celiac disease)
-
Eyes
- Conjunctivitis
- Episcleritis (Crohn's Disease)
-
Mouth
- Aphthous Ulcers (Crohn's Disease, Gluten Sensitivity)
- Glossitis (Vitamin B12, Iron, folate and niacin deficiency)
- Angular kuelos (vitamin B12, iron, folate and niacin deficiency)
- Dental Hypoplasia (Gluten Sensitivity)
-
Hands
- Raynaud's phenomenon (Scleroderma)
- Drumstick fingers (Crohn's disease, lymphoma, EIPID)
- Coilinoquia (Iron Deficiency)
-
Musculoskeletal apparatus
- Mono / polyarthropathies: (Crohn's disease, gluten sensitivity, Whipple's disease, Behcet's disease)
- Back pain due to osteoporosis: (Crohn's diseases, malnutrition, Celiac diseases)
- Muscle weakness from low levels of K, magnesium and vitamin D: (lymphoma, bacterial overgrowth)
-
Nervous system
- Peripheral neuropathy: (vitamin B12 deficiency due to pernicious anemia or bacterial overgrowth)
- Central: seizures, cranial nerve palsy (Whipple's disease, gluten sensitivity, diffuse lymphoma)
Study Methodology
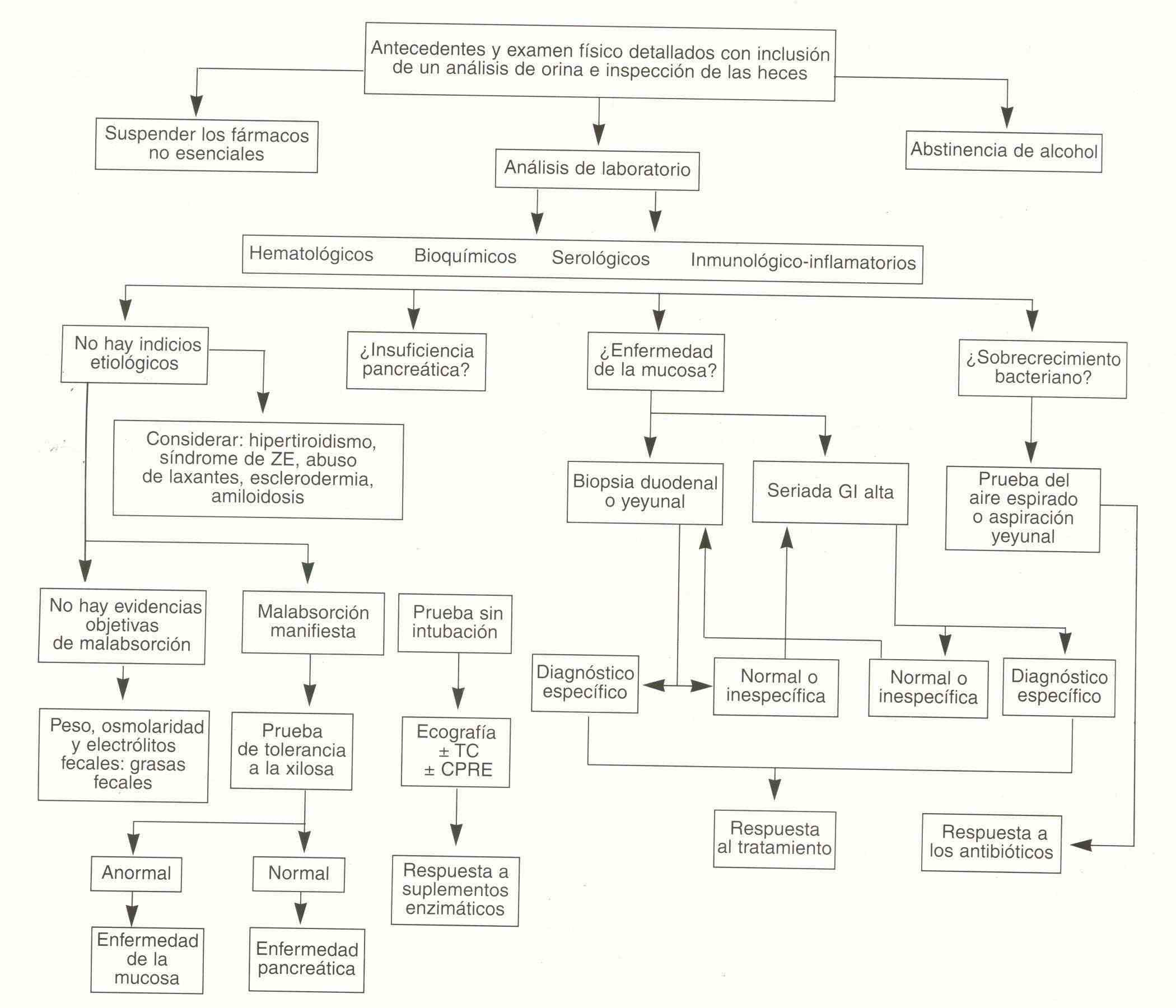
Because the Bad Absorption Syndrome encompasses the clinical manifestation of multiple pathologies, it is that with the symptoms and signs it is not always possible to reach the etiological diagnosis, so it is necessary to have an order in the analysis of these patients, so it is It is useful to follow an algorithm to ensure that all possibilities are evaluated.
Normal characters of stool:
The normal amount of stool produced by a healthy adult man with a balanced diet is 100 to 200 g / day. In the case of a diet rich in fiber, its volume increases. The dry weight is 66 grams.
The color is dark brown, darker with a diet rich in meat, and lighter with an abundant intake of dairy products. The variable consistency within certain limits, and the sui generis smell. The intestine is usually evacuated once a day.
On microscopic examination of fecal matter with a full diet, isolated remains of muscle fibers, fatty acids combined with Ca ++ in the form of crystalline masses, and vegetable remains of oats and bread can be found. In the chemical examination it is possible to find fats of 2.5 to 4.5 g / day, free fatty acids of 0.01 to 0.10 g / day (1 to 10% of the dry fecal matter) and combined as soap 0.005 to 0.12 g / day (0.5 to 12% of dry fecal matter) and nitrogen from 0.80 to 1.60 g / day; the protein content is minimal. The pH ranges from 6.8 to 7.3. in intestinal fermentation with a diet rich in carbohydrates the reaction is acidic; in rot with a diet rich in protein, in pH it is alkaline.
Stool Study Procedures
A very practical method to evaluate the fat content in stool is the microscopic examination of a sample of the same stained with Sudan III that correlates well with the van de Kamer test, which is the most reliable, although cumbersome, method for define a steatorrhea.
The van de Kamer test consists of administering a diet of 100 grams of fat from different sources per day for six days. Fat in stool should not exceed 5-6 grams in the day.
The labeled triolein oral 14C is a method for evaluating the absorption of fat. Ingested C14 triolein is hydrolyzed in the digestive tract and C14 glycerol is absorbed and metabolized in the liver. The C14 of the CO2 produced is exhaled and can be measured.
D-xylose absorption is the most widely used method to assess carbohydrate absorption. After ingesting 25 grams of D-xylose, its urinary elimination is measured in the course of five hours after its administration. Normally 4 or more grams are excreted in that period. Excretion is less with proximal small bowel disorders such as tropical and non-tropical sprue.
The Schilling test is used to evaluate the absorption of vitamin B12. 1000 Mg are injected. of vitamin B12 intramuscularly to saturate the body's deposits in order to avoid that a depletion of them could fix the ingested vitamin and prevent its urinary elimination. A dose of 57 Co-labeled vitamin B12 is ingested and urine is collected for the next 48 hours. In this period, at least 8% of the administered radioactivity must be eliminated. The test can be performed with or without the administration of intrinsic factor and with or without simultaneous treatment with antibiotics. In the case of low figures that are normalized with intrinsic factor, it is atrophic gastritis; normalization with antibiotics speaks of bacterial overgrowth.
The presence of leukocytes in the stool indicates the existence of an inflammatory diarrhea, just as that of eosinophils suggests an eosinophilic enteritis or parasitosis. The investigation of hidden blood in fecal matter by the guaiac or benzidine method guides the search for an organic pathology.
The secretin test is used to detect diffuse pancreatic insufficiency. It is administered intravenously as a bolus or drip, and the concentration of pancreatic enzymes in the duodenal contents is measured. A volume greater than 1.8 ml / kg / h and a bicarbonate concentration greater than 80 mEq / l is normal.
The blood levels of albumin, cholesterol, calcium, magnesium, Fe, transferrin, vitamin B folic acid, vitamin A, carotenes, may be decreased according to the symptoms and its pathophysiology. Prolonged prothrombin time is likely to be found in vitamin K deficiencies. Oral glucose tolerance test may be flat.
Culture of the duodenal contents should not show a number of colonies greater than per milliliter. The presence of higher numbers indicates bacterial overgrowth.
The search for parasites in feces and stool culture are in common use. All patients in whom malabsorption is suspected should be radiologically studied in their digestive tract in search of characteristic signs: barium flocculation, fragmentation and segmentation, thickening and nodular folds in the duodenum, and dilations in the small intestine, in addition to specific lesions such as fistulas, gastroileostonomy, tumors, etc. The time of intestinal passage can be measured by the ingestion of barium, which reaches the cecum in a period of 3 to 5 hours and the rectum in 24 hours.
The dosage of a1-antitrypsin blood and stool used to evaluate the existence of a protein losing enteropathy.
The intestinal biopsy thin is useful in the differential diagnosis of malabsorption syndrome, such as Whipple's disease. In segmental pathologies such as regional enteritis, lymphoma or eosinophilic enteritis, its value depends on the biopsied area.
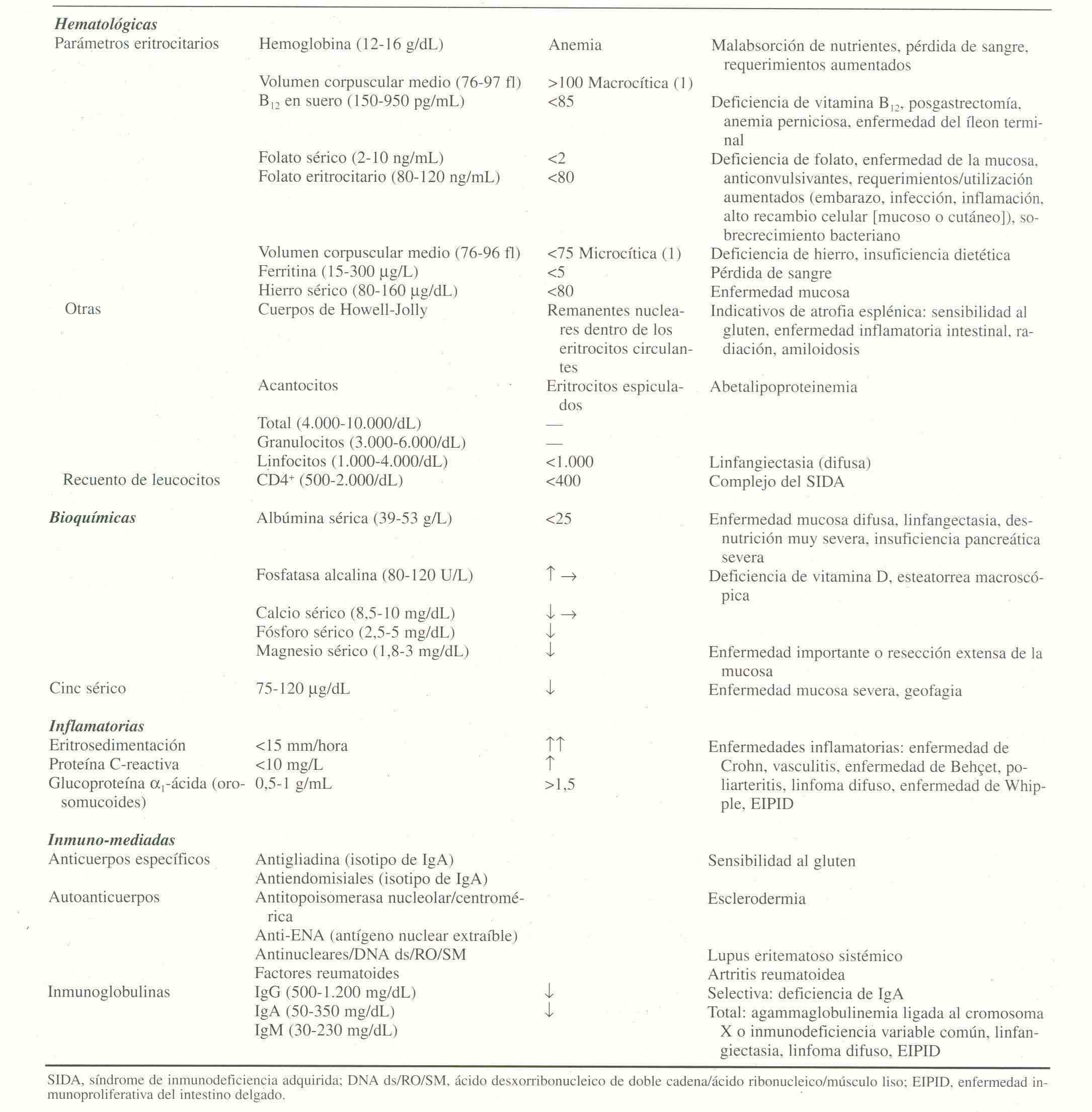
The laboratory analysis should include the hematological, biochemical serological and inflammatory immunological study